Generic Medications: What They Are, How They Work, and What You Need to Know
When you hear generic medications, pharmaceutical products that contain the same active ingredients as brand-name drugs but are sold without a brand name. Also known as generic drugs, they are legally required to work the same way as their brand-name counterparts — same dose, same route, same effect. But here’s the catch: they don’t always behave the same in your body. That’s not because they’re fake. It’s because of how they’re made.
Behind every generic drug, a non-brand version of a medication approved by the FDA as bioequivalent to the original is a complex process. The FDA requirements, strict standards set by the U.S. Food and Drug Administration to ensure generic drugs are safe, effective, and consistent demand that these drugs match the brand in strength, purity, and performance. But stability testing, manufacturing defects, and even tiny differences in inactive ingredients can change how your body absorbs the drug. That’s why some people notice side effects or reduced effectiveness after switching — especially with narrow therapeutic index, a category of drugs where small changes in blood levels can lead to treatment failure or serious toxicity medications like warfarin, levothyroxine, or lamotrigine.
Not all generic drugs are created equal. Some are made in factories with outdated equipment. Others face contamination issues, capping defects, or inconsistent dosing. The FDA catches many of these problems — but not all. And when it comes to drugs where a 10% difference in absorption can mean the difference between control and crisis, that’s not just a technicality. It’s a health risk. That’s why 27 states have laws blocking automatic substitution for these critical meds. It’s also why pharmacists are now trained to spot fake pills, why expiration tracking matters more than ever, and why your doctor needs to know if you’ve switched generics.
What you’ll find below isn’t just a list of articles. It’s a practical guide to navigating the real world of generic medications — from how they’re tested and approved, to when you should insist on staying with the brand, to how to avoid waste, detect defects, and talk to your pharmacist about safety. Whether you’re saving money on insulin, managing epilepsy with antiseizure drugs, or just trying to make sense of a new pill bottle, these posts give you the facts you need — no fluff, no marketing, just what works.
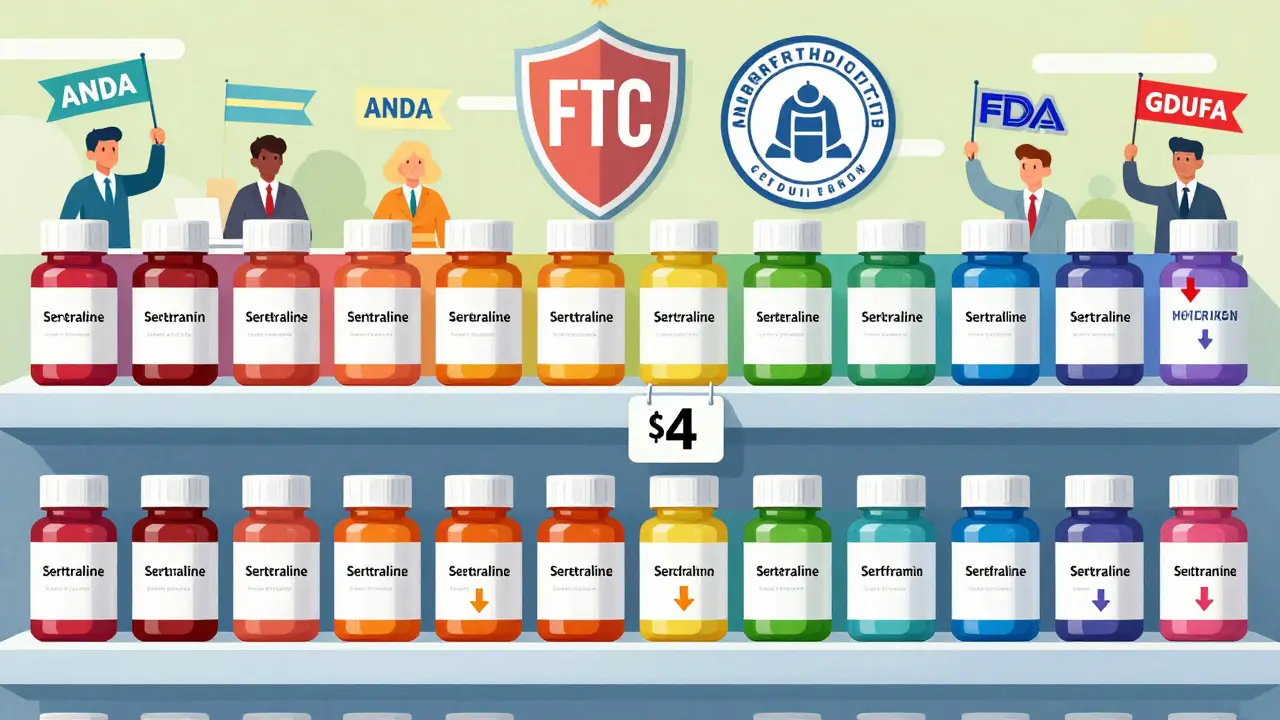
Generic drugs make up 90% of U.S. prescriptions but only 23% of drug spending. Learn how competition, not government price controls, keeps them affordable-and why policymakers focus on blocking anti-competitive behavior instead.
Jan, 22 2026
Clinician communication is the most powerful factor in whether patients accept generic medications. Clear, confident explanations about FDA bioequivalence, cost savings, and safety can reduce skepticism, improve adherence, and save billions in healthcare costs.
Dec, 1 2025