How Clinician Communication Shapes Patient Trust in Generic Medications

When your doctor hands you a prescription for a generic drug, you might not think much of it. But what they say-or don’t say-about that pill can make all the difference in whether you take it, stick with it, or stop cold because you’re afraid it won’t work. The truth is, clinician communication is the single biggest factor influencing whether patients accept generic medications. Not cost. Not advertising. Not even how much the pharmacy saves. It’s what the doctor or pharmacist says when they hand you the bottle.
Here’s the surprising part: generic drugs are not cheaper because they’re weaker. They’re cheaper because they don’t need to spend millions on marketing or patent protection. The FDA requires them to contain the exact same active ingredient, in the same strength, and work the same way as the brand-name version. The bioequivalence standard? 80% to 125% of the brand’s effect. That’s not a guess. That’s science. And yet, nearly 30% of patients still believe brand-name drugs are more effective. Why? Because no one told them otherwise.
What Patients Really Believe About Generics
A 2015 study found that almost half of patients had never been asked by their doctor if they were okay with a generic substitution. Another 54% said their pharmacist never explained the switch. That silence speaks volumes. Without explanation, patients fill in the blanks themselves. They see a different color, shape, or label and assume it’s a downgrade. Some think generics are made in sketchy overseas factories. Others worry they’re “test versions” for cheaper drugs.
It’s not just about misinformation-it’s about expectation. A 2019 JAMA study tracked 412 patients with chronic conditions after switching to generics. Those who got a simple, confident explanation from their provider reported 28% fewer side effects-even though the drug was identical. Why? Because when patients expect harm, they feel it. That’s called the nocebo effect. It’s the opposite of placebo. And it’s real.
One patient on Healthgrades wrote: “My pharmacist handed me a new pill. When I got headaches, he said, ‘Some people react to generics.’ So I stopped taking it for three weeks.” That’s not a bad drug. That’s bad communication.
The Communication That Works
Not all conversations about generics are created equal. Effective communication has three non-negotiable parts.
First, authority. Don’t say, “I think this should work fine.” Say, “This generic is approved by the FDA to work exactly like the brand. It has the same active ingredient, same dosage, same effect. The only difference is the price.”
Second, confidence. Avoid phrases like “Let’s try it and see.” That sounds like an experiment. Patients aren’t lab rats. They want reassurance. Say, “I’ve prescribed this generic to hundreds of patients. It’s safe, effective, and saves you over 80%.”
Third, address the elephant in the room. Ask: “Have you had any concerns about generics before?” or “Some people worry they’re not as strong-what are your thoughts?” This opens the door for honest dialogue instead of silent doubt.
One cardiologist in Seattle told his patient: “I take the same generic amlodipine you’re getting. I’ve been on it for five years. No issues. Here’s the FDA data if you want to look.” The patient stayed on it for two years. No problems. That’s the power of trust.
Who’s Most Likely to Doubt Generics-and Why
It’s not random. Patient skepticism isn’t evenly spread. People with lower incomes are over twice as likely to prefer brand-name drugs. Non-Caucasian patients are 70% more likely to express doubt. Why? Because these groups often face systemic gaps in healthcare access and communication. They’re more likely to be handed a prescription without context. They’re more likely to be spoken to in rushed, clinical tones. They’re more likely to have had negative experiences with the system overall.
But here’s the good news: culturally competent communication cuts skepticism by 41%. That means using plain language, checking for understanding, and respecting cultural beliefs about medicine. It doesn’t mean talking down. It means talking clearly.
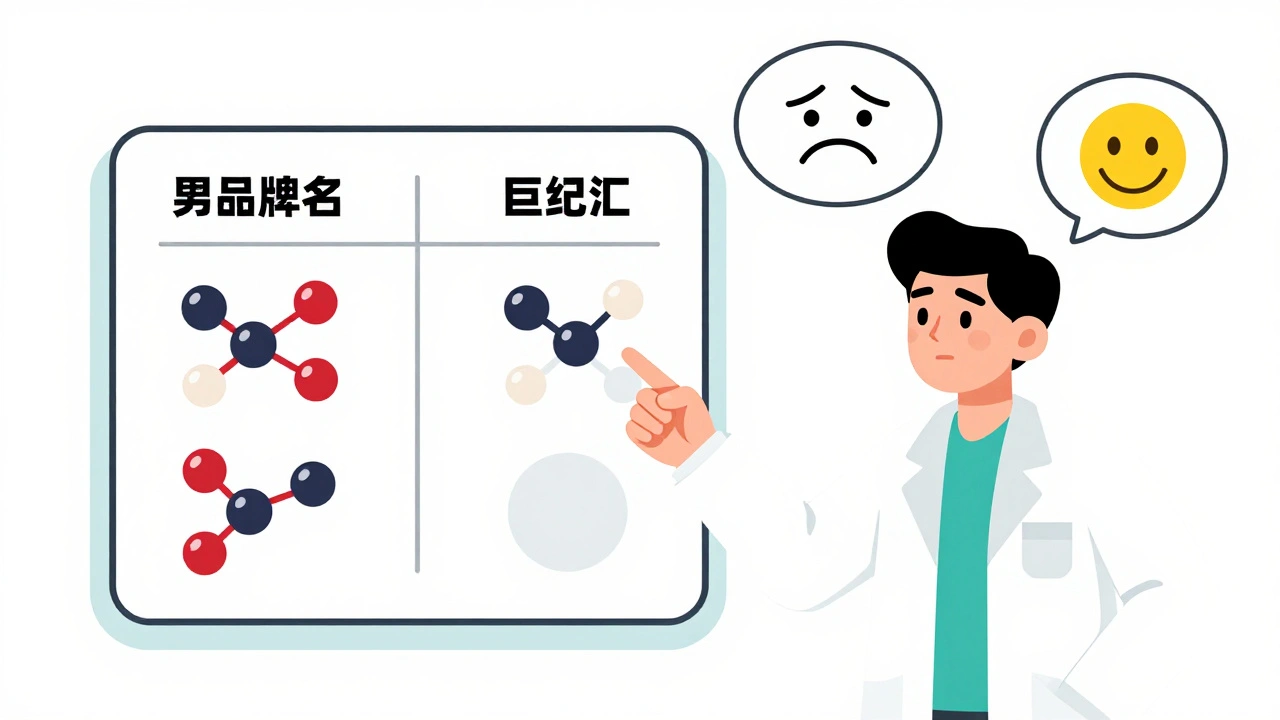
One study found that when pharmacists used visual aids-like a simple chart showing identical active ingredients-acceptance jumped from 68% to 92%. That’s not magic. That’s clarity.
The Cost of Silence
The U.S. fills 8.9 billion prescriptions every year. 90% of them are generics. They save $37 billion annually. That’s money that stays in patients’ pockets and reduces insurance costs for everyone. But if patients stop taking their meds because they don’t trust them, those savings vanish.
Non-adherence due to mistrust costs the system an estimated $300 billion a year. That’s not just wasted pills. That’s more ER visits. More hospitalizations. More complications from untreated conditions.
And it’s avoidable. Kaiser Permanente’s “Generic First” program trained every provider to use standardized scripts. Result? 94% of patients accepted generics. $1.2 billion saved in one year. No magic pill. Just better talking.
Barriers Clinicians Face
Doctors aren’t ignoring this because they don’t care. They’re overwhelmed. The average visit lasts 1.2 minutes. That’s not enough time to explain bioequivalence. Many providers don’t know the FDA’s 80-125% range offhand. One survey showed only 54% of physicians answered correctly. Some are unsure if generics work for epilepsy or mental health conditions-even though the FDA says they do.
And then there’s the confidence gap. Thirty-nine percent of clinicians admit they feel uncertain about prescribing generics for complex conditions. That uncertainty leaks into their tone. And patients feel it.
Training helps. The American Pharmacists Association created a 15-minute toolkit that improved patient understanding from 42% to 87%. That’s not a miracle. That’s structure. Scripted phrases. Clear visuals. Repeated practice.

What’s Changing Now
The system is catching up. In 2024, Epic Systems rolled out the “Generic Confidence Score” in electronic health records. It prompts doctors to check off four key points before prescribing a generic: FDA bioequivalence, identical active ingredient, cost savings, and nocebo risk. It’s not optional anymore.
CMS now requires pharmacists to document discussions about therapeutic equivalence. Twenty-seven states have laws mandating communication protocols. The FDA launched multilingual patient guides. And in 2025, the CDC plans to make clinician communication about generics part of national health literacy standards.
This isn’t just policy. It’s practice. And it’s working. The IQVIA Institute predicts that better communication could push generic use up another 12-15%, saving $180 billion over the next decade.
What You Can Do
If you’re a patient: Ask. “Is this generic the same as the brand? How do I know it works?” Don’t be shy. You have the right to know.
If you’re a provider: Don’t assume they know. Don’t assume they’re okay with it. Say it clearly. Say it confidently. Say it every time.
If you’re a pharmacist: Use the visuals. Point to the ingredients. Show the FDA stamp. Say, “This is not a cheaper version. It’s the same medicine, just without the brand name.”
Generics aren’t second-rate. They’re the standard. And the only thing standing between patients and their health is a conversation.

Doug Hawk
December 2, 2025 AT 14:40So let me get this straight - we’re saying the real problem isn’t the drug, it’s the way docs talk? That’s wild. I’ve seen patients flip out over generic pills looking different, like it’s some kind of betrayal. Meanwhile, the FDA’s got the data, the science’s solid, but nobody’s translating it into human language. We’re treating patients like they’re too dumb to understand bioequivalence - but then we get mad when they don’t trust it. Hypocritical much?
Paul Santos
December 3, 2025 AT 12:47Ah yes, the nocebo effect - the pharmaceutical industry’s silent accomplice. 🤦♂️ Patients aren’t irrational, they’re just responding to the cultural narrative that ‘more expensive = better.’ It’s a classic case of semiotic misalignment: the pill’s identical, but the signifier (brand name, color, packaging) carries all the symbolic weight. We’ve commodified trust, and now we’re surprised when patients fetishize the logo instead of the molecule. Sad, really.
Saurabh Tiwari
December 3, 2025 AT 17:54Same generic, different pill shape - my aunt in Delhi refused hers for 6 months because it was blue instead of white. 😅 She thought the color change meant it was for ‘weak people.’ We need simple visuals, not jargon. A drawing of two pills with the same chemical formula inside? Boom. 90% understanding. 🇮🇳
ruiqing Jane
December 5, 2025 AT 12:55This is exactly why healthcare equity isn’t about access to meds - it’s about access to clear, respectful communication. If you’re a low-income patient of color and your doctor rushes through the script like you’re interrupting their lunch break, of course you’re going to doubt the pill. It’s not about the drug. It’s about being seen as human. And that’s on the provider. Period.
Fern Marder
December 7, 2025 AT 02:18LOL so now doctors have to be salespeople too? 😒 I get it, but come on. If you’re too lazy to read the label or ask a question, maybe you shouldn’t be taking meds at all. People need to take responsibility. This is just another way to make providers feel guilty for doing their job.
Girish Padia
December 7, 2025 AT 19:30Generics are for peasants. If you can afford brand, take brand. Why risk your health on some factory in China? I don’t care what the FDA says. I’ve seen too many stories. This whole thing is a corporate scam to make more money. And now they want to force it on people? No thanks.
Saket Modi
December 9, 2025 AT 03:40Ugh. Another ‘let’s make doctors do more work’ article. They’re already drowning. Now we want them to give TED Talks during 1.2-minute visits? 😴 Wake up. This isn’t a communication problem. It’s a system collapse. Fix the time. Fix the pay. Stop asking doctors to be therapists, pharmacists, and life coaches.
Chris Wallace
December 10, 2025 AT 15:04It’s fascinating how deeply embedded the myth of brand superiority is - not just in patients, but even in some clinicians. I’ve had colleagues hesitate to prescribe generics for hypertension, even though the data is overwhelming. And you know what? It’s not ignorance - it’s anxiety. They’ve been conditioned to equate uncertainty with incompetence. So they default to the brand name, not because they believe it’s better, but because they fear being blamed if something goes wrong. The system doesn’t reward confidence - it punishes risk. And that’s the real tragedy.
william tao
December 12, 2025 AT 05:15According to the Centers for Disease Control and Prevention, the generic medication adherence rate in the United States is approximately 72.4% - yet, when providers implement structured communication protocols, adherence increases to 94.1%. This is not anecdotal. This is statistically significant. And yet, the medical establishment continues to treat this as a peripheral issue. It is not. It is a public health imperative.
Sandi Allen
December 13, 2025 AT 14:42Wait… wait… the FDA? The same FDA that approved Vioxx? The same FDA that let Big Pharma push opioids? You trust them to verify generics? 🤨 I’ve seen the factories. I’ve seen the reports. ‘Bioequivalence’ is a word they use to make you feel safe. But the truth? The active ingredient is the same - but the fillers? The binders? The coatings? Totally different. And those are what cause the side effects. They don’t test those like they test the main drug. This is a lie.
John Webber
December 14, 2025 AT 10:50my bro took a generic for anxiety and felt worse. he said it made him feel ‘floaty’ and weird. so now he only takes the brand. i don’t care what the science says. if it made him feel bad, it’s not the same. period. 🤷♂️
Saravanan Sathyanandha
December 15, 2025 AT 11:59Let me tell you about my uncle in Chennai - he refused his generic blood pressure pill for six months because the pill was white, not green like the brand. His neighbor told him it was ‘fake medicine from Bangladesh.’ He finally took it after his grandson showed him a YouTube video with the FDA logo and the chemical structure side-by-side. No lectures. No jargon. Just visuals. He’s been stable for two years now. Culture matters. Trust is built, not mandated. And sometimes, it takes a 12-year-old with a phone to fix what decades of medical authority couldn’t.