Voriconazole Liver Risk: What You Need to Know About Liver Damage and Safe Use
When you take voriconazole, a powerful antifungal used for serious fungal infections like invasive aspergillosis. Also known as Vfend, it saves lives—but it can also hurt your liver. This isn’t a rare side effect. Studies show up to 1 in 5 people on voriconazole develop signs of liver stress, and some end up with serious, even life-threatening damage. If you’re on this drug, you need to know the signs, the risks, and what to do next.
The liver doesn’t scream when it’s in trouble. Instead, it whispers—through fatigue, yellow eyes, dark urine, or nausea that won’t go away. These aren’t just "bad days." They’re red flags tied to drug-induced liver injury, a known pattern with voriconazole where the body’s metabolism turns the drug into toxic byproducts. Your doctor should check your liver enzymes before you start, then every week or two during treatment. If ALT or AST levels jump more than 3 times above normal, they’ll likely pause the drug. No waiting. No hoping it gets better. That’s the standard for a reason.
Some people are more at risk. Older adults, people with existing liver disease, or those taking other meds that strain the liver—like statins, antiseizure drugs, or even some antibiotics—face higher danger. voriconazole monitoring, the routine blood tests that track liver function isn’t optional. It’s your safety net. Skipping it because you feel fine is like driving without checking your brakes. You might be okay today, but the next dose could be the one that pushes you over the edge.
And it’s not just about the drug itself. Your genes matter. Some people have a slower version of the CYP2C19 enzyme, which breaks down voriconazole. That means the drug builds up in your blood, raising the chance of liver damage. If you’ve had bad reactions to other antifungals or meds before, tell your doctor. They might adjust your dose or pick a different drug entirely.
You don’t have to choose between fighting a deadly infection and risking your liver. But you do need to be active. Track your symptoms. Know your blood test results. Ask if there’s a safer alternative. And never stop or start a dose without talking to your care team. The goal isn’t just to kill the fungus—it’s to keep your body working while you do it.
Below, you’ll find real stories and practical advice from people who’ve walked this path—what worked, what didn’t, and how to spot trouble before it’s too late.
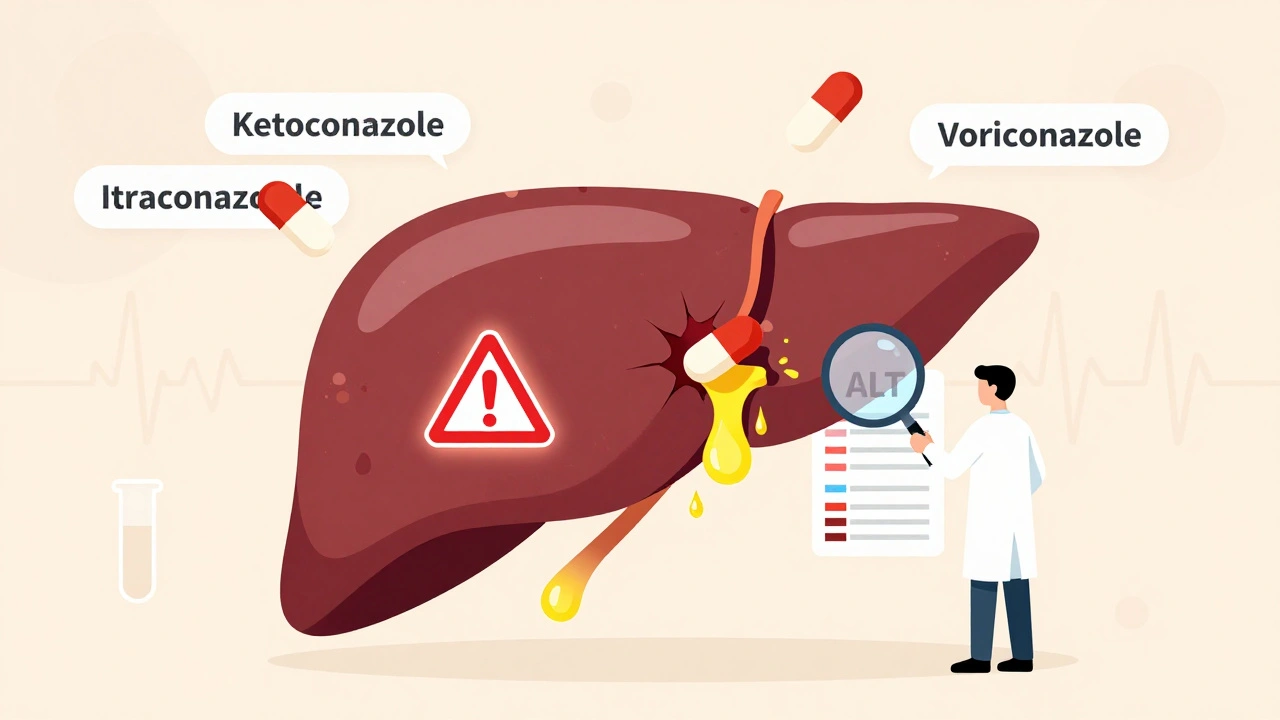
Antifungals can cause serious liver damage, especially ketoconazole, itraconazole, and voriconazole. Learn which drugs are riskiest, how to spot early signs of liver injury, and what monitoring you need to stay safe.
Dec, 2 2025