Antifungals: Liver Safety and Drug Interaction Risks You Can't Ignore
When you take an antifungal for a stubborn nail infection or a systemic yeast problem, you’re not just fighting fungus-you’re putting your liver on the line. Most people assume these drugs are safe because they’re common, over-the-counter, or prescribed by a doctor. But the truth is, some antifungals carry a real risk of serious liver damage, and the warning signs often show up too late.
Why Your Liver Is at Risk
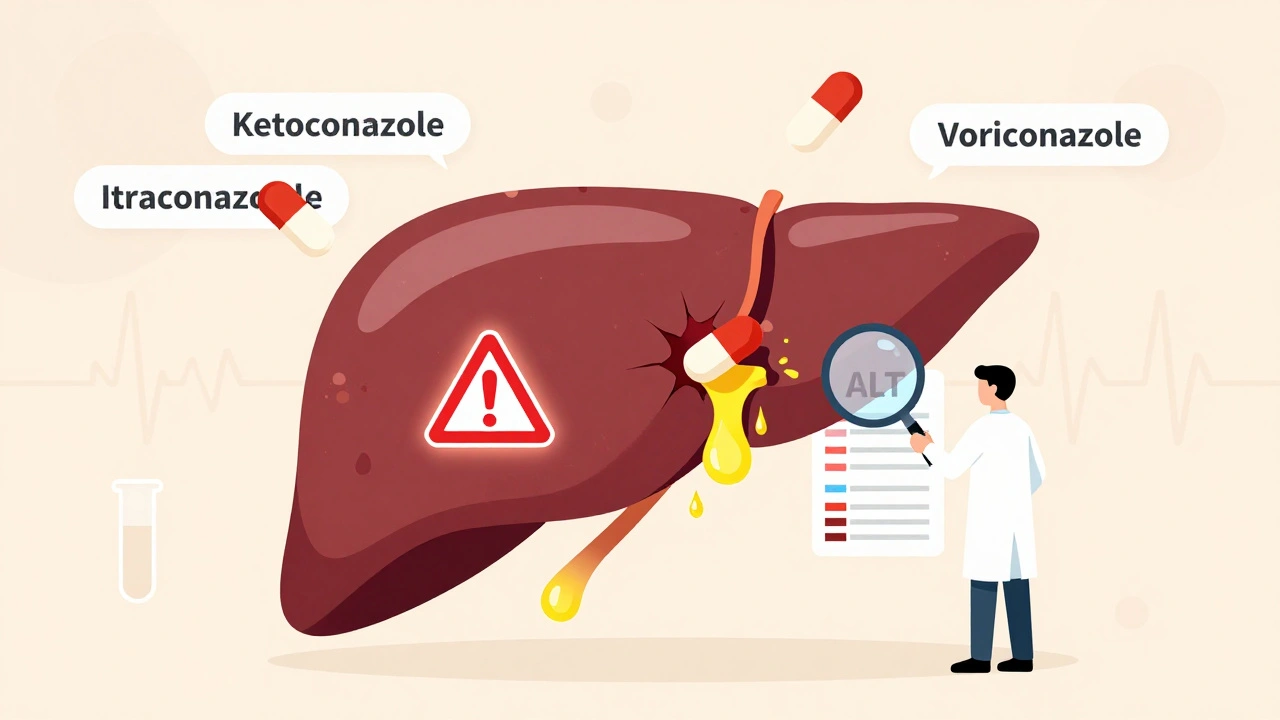
Antifungals don’t just target fungi. They mess with your liver’s ability to process chemicals, and that’s where things go wrong. The liver breaks down these drugs, but some antifungals are so harsh on liver cells that they cause inflammation, cell death, or even complete failure. It’s not rare. Between 2004 and 2021, the FDA recorded over 4,000 reports of liver injury linked to antifungal use. The real number is likely higher-many cases go unreported because symptoms like fatigue or nausea are easy to ignore.The Worst Offenders: Ketoconazole, Itraconazole, Voriconazole
Not all antifungals are created equal. Some are far more dangerous to your liver than others. Ketoconazole used to be the go-to oral antifungal. Now, it’s a last-resort drug. The FDA slapped it with a boxed warning in 2013-its strongest alert-after linking it to over 1,800 cases of liver injury. One patient in a Reddit thread saw their ALT levels spike to 1,200 U/L (normal is under 56). That’s liver failure territory. Doctors in Europe stopped prescribing it entirely in 2013. In the U.S., it’s only used when nothing else works, and even then, only if your liver is already healthy. Itraconazole and voriconazole are next in line. A 2009 meta-analysis found these two caused liver injury more often than fluconazole. Voriconazole is especially tricky because it’s used in cancer and transplant patients-people already at higher risk. Studies show that if you have a certain gene variation (CYP2C19), your risk of liver damage from voriconazole jumps nearly fourfold. That’s why some hospitals now test for this before prescribing it.The Misunderstood Safe Ones: Terbinafine and Echinocandins
Many assume terbinafine (used for athlete’s foot and nail fungus) is harmless because it’s available over the counter. But it carries a black box warning from the FDA for rare but deadly liver failure. The risk is low-about 1 in 1,000-but it strikes fast. Most cases happen within the first six weeks. A 2023 Healthline user reported jaundice at week five. They stopped the drug and recovered, but not everyone is that lucky. Then there are the echinocandins-caspofungin, micafungin, and anidulafungin. These are given intravenously in hospitals for serious infections like candidemia. You’d think they’d be safer since they’re not processed by the liver the same way. But data from the FDA shows anidulafungin had the highest death rate among DILI cases-50%. That sounds terrifying, but here’s the catch: these drugs are usually given to people who are already critically ill, often with pre-existing liver damage. So the risk isn’t necessarily from the drug itself-it’s from the patient’s condition. Micafungin has the best safety profile among this group.
How to Spot Trouble Before It’s Too Late
Liver damage doesn’t always show up on a blood test right away. Early signs are vague: fatigue, nausea, loss of appetite, dark urine, or yellowing of the skin. By the time you feel sick, your liver might already be badly hurt. The good news? You can catch it early with simple blood tests. Here’s what experts recommend:- Baseline test: Get liver function tests (ALT, AST, bilirubin) before starting any systemic antifungal.
- Weekly monitoring: For ketoconazole, itraconazole, and voriconazole, check every week for the first month.
- Biweekly after that: Keep checking every two weeks if you’re on long-term therapy.
- Terbinafine: Test at 4-6 weeks, then again if you’re on it longer than 8 weeks.
Stop the drug if:
- ALT or AST is more than 3 times the normal level AND you have symptoms like nausea or jaundice.
- ALT or AST is more than 5 times normal-even if you feel fine.
That’s not a suggestion. That’s the standard of care.
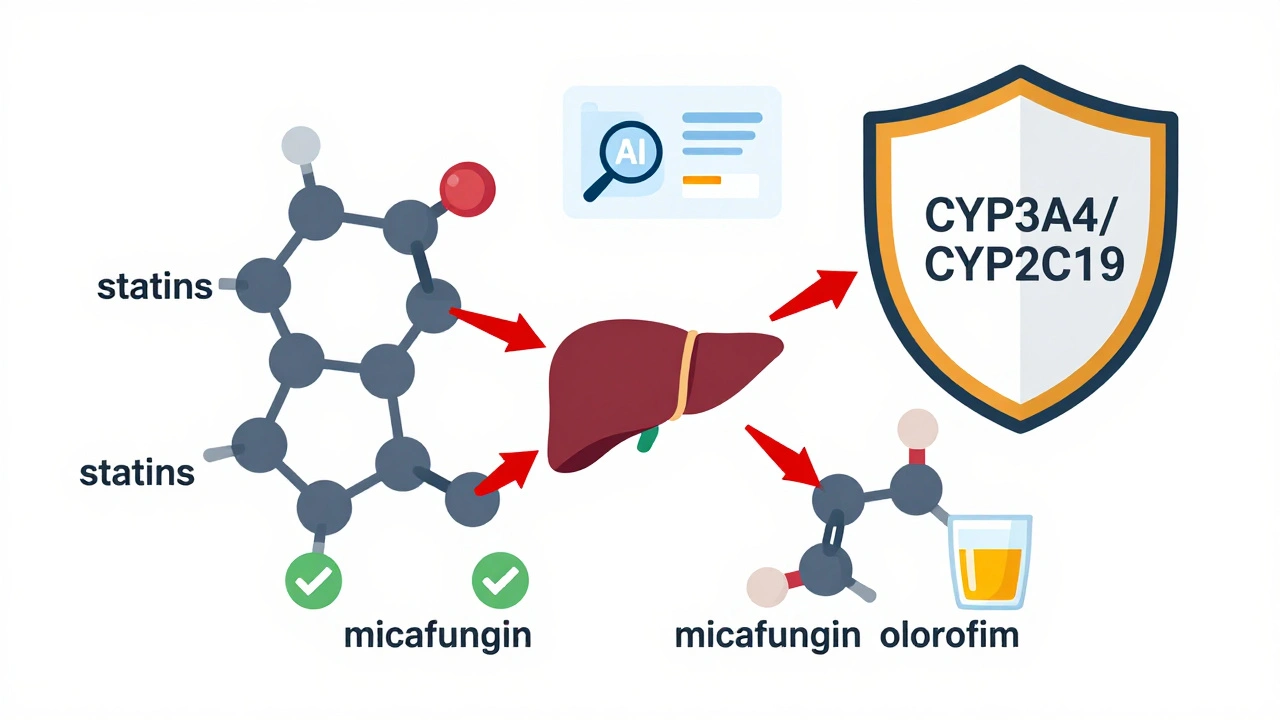
Drug Interactions: The Hidden Danger
Antifungals don’t just hurt your liver-they make other drugs more dangerous. Many antifungals block liver enzymes (CYP3A4, CYP2C19) that break down other medications. This causes those drugs to build up in your system. Here are common and dangerous combos:- Voriconazole + statins: Can cause muscle breakdown (rhabdomyolysis), which can lead to kidney failure.
- Itraconazole + blood thinners (warfarin): Increases bleeding risk dramatically.
- Fluconazole + diabetes drugs: Can cause dangerous drops in blood sugar.
- Any azole + alcohol: Increases liver stress and risk of injury.
Always tell your doctor every medication, supplement, or herb you take-even CBD or St. John’s Wort. Many people don’t realize these can interact too.
Who’s Most at Risk?
You’re not equally at risk. Certain people need extra caution:- People over 65: Liver function slows with age. Risk of injury is over 7 times higher than in younger adults.
- Those with existing liver disease: Hepatitis, fatty liver, or cirrhosis? Avoid ketoconazole entirely. Even terbinafine needs careful monitoring.
- People on multiple medications: The more drugs you take, the higher the chance of a bad interaction.
- Those with genetic differences: If you’re a slow metabolizer of CYP2C19, voriconazole is riskier. Genetic testing is now available and worth considering.
What’s Changing in 2025?
The field is evolving fast. Ketoconazole use has dropped by over 90% since 2013. Hospitals now use echinocandins as first-line for invasive candidiasis-not because they’re perfectly safe, but because they’re safer than azoles for most patients. New antifungals like olorofim and ibrexafungerp are in development. Early trials show they cause 78% fewer liver enzyme spikes than older azoles. That’s huge. The FDA is also using AI to scan adverse event reports in real time, hoping to catch liver risks before they become widespread.And for the first time, pre-treatment genetic testing for CYP2C19 is being recommended in some major hospitals. It’s not routine yet-but it might be soon.
What You Should Do Now
If you’re on or thinking about starting an antifungal:- Ask your doctor: “Which one are you prescribing, and why?”
- Request a baseline liver test before you start.
- Ask if you need weekly blood work-and stick to it.
- Never take antifungals with alcohol or other liver-stressing drugs without checking.
- If you feel unusually tired, nauseous, or notice yellowing skin, stop the drug and get tested immediately.
Don’t assume your doctor knows all the risks. Many primary care providers don’t monitor LFTs for terbinafine, even though the guidelines say they should. A 2020 study found only 37% of them did it right. Be your own advocate.
Antifungals save lives. But they can also end them-quietly, and without warning. The difference between safety and disaster often comes down to one simple thing: paying attention to your liver.
Can antifungals cause permanent liver damage?
Yes, in rare cases. While most people recover fully after stopping the drug, some develop acute liver failure that requires a transplant. Ketoconazole has been linked to multiple transplant cases. Terbinafine and voriconazole have also caused irreversible damage in patients who didn’t get timely monitoring. Early detection is the only way to prevent permanent harm.
Is fluconazole safer than other azoles?
Yes, fluconazole has the lowest risk of liver injury among the azoles. Studies show it causes liver damage in less than 0.1% of users, compared to 0.5-1% for itraconazole and voriconazole. It’s still not risk-free-especially in people with existing liver disease or those on long-term therapy-but it’s the safest oral azole option when appropriate.
Should I avoid terbinafine for nail fungus?
Not necessarily. Terbinafine is still the most effective treatment for fungal nail infections. But you should get a liver test before starting and again at 4-6 weeks. If you have a history of liver disease, drink alcohol regularly, or take other medications that affect the liver, your doctor may recommend a different treatment. The risk is low, but the consequences are serious enough to warrant caution.
Why is ketoconazole still available if it’s so dangerous?
It’s only approved for rare, life-threatening fungal infections like endemic mycoses (e.g., blastomycosis, histoplasmosis) when other drugs won’t work or aren’t available. It’s no longer used for acne, dandruff, or routine fungal infections. The FDA restricted it in 2013 because safer alternatives exist. If your doctor prescribes it for anything else, ask why.
Can I drink alcohol while taking antifungals?
No. Alcohol stresses the liver, and antifungals already do that. Combining them increases your risk of liver injury significantly-even with drugs considered safer like fluconazole. Avoid alcohol completely during treatment and for at least a week after stopping.
What if my liver enzymes are high but I feel fine?
Don’t ignore it. Many people with serious liver injury have no symptoms at first. If your ALT or AST is over 5 times the upper limit of normal, your doctor should stop the antifungal immediately-even if you feel okay. Waiting for symptoms means waiting too long.

parth pandya
December 3, 2025 AT 16:20man i just started terbinafine last week for my toenail thing and didnt even know about the liver risk
got my bloodwork done yesterday and alt was 48… still in range but now im paranoid
why dont more people talk about this
Albert Essel
December 4, 2025 AT 11:54This is one of the most well-researched and urgently needed posts I’ve seen on this topic. The breakdown of each antifungal’s risk profile, paired with actionable monitoring guidelines, should be mandatory reading for anyone prescribed these drugs. Thank you for compiling this with such precision.
Charles Moore
December 5, 2025 AT 03:39Really appreciate you laying this out so clearly. I’m a nurse in a rural clinic and I’ve seen too many patients ignore the fatigue or brush off dark urine as ‘just dehydration.’
Now I print out this exact list and hand it to them. Simple. No jargon. Just facts. If we can catch one case early because of this, it’s worth it.
Gavin Boyne
December 6, 2025 AT 21:31So let me get this straight - we’re telling people to get weekly liver tests for drugs that cost $20 and are sold over the counter, while we let them take opioids with zero monitoring?
Our healthcare system is a circus, and the clowns are prescribing antifungals like they’re vitamins.
Also, fluconazole is safer? Cool. Now tell me why my insurance won’t cover it unless I fail terbinafine first. 😌
Rashi Taliyan
December 8, 2025 AT 06:08OMG I just had to stop terbinafine after 5 weeks because my skin turned yellow 😭
I thought it was just sunburn…
My mom screamed when she saw me - I looked like a lemon
Thank you for writing this. I would’ve kept taking it until I collapsed.
PLEASE tell everyone. This is not a joke.
Kara Bysterbusch
December 9, 2025 AT 16:58While the clinical data presented here is both compelling and statistically robust, I must emphasize the epistemological imperative of patient autonomy in the context of pharmacovigilance. The implicit assumption that patients are passive recipients of medical authority must be critically interrogated. Informed consent, when contextualized within the socio-ecological determinants of health, becomes not merely a procedural formality but a moral covenant. This post, in its meticulous articulation of risk stratification, exemplifies the highest standard of ethical pharmacological communication.
Francine Phillips
December 9, 2025 AT 19:47yeah i guess liver is a thing
but i took it for 3 months and felt fine so whatever
Katherine Gianelli
December 10, 2025 AT 19:39Reading this made me so glad I asked my doctor for the bloodwork before starting fluconazole. I was nervous, but I’m so glad I did.
And hey - if you’re on this stuff, don’t feel dumb for asking questions. Your liver doesn’t care how ‘basic’ your question sounds. It just wants you to pay attention.
You got this. Seriously.
Joykrishna Banerjee
December 10, 2025 AT 22:46Of course the FDA didn’t ban ketoconazole outright - because the pharmaceutical-industrial complex thrives on reactive regulation, not proactive prevention. The real tragedy? The CYP2C19 polymorphism data has been available since 2007, yet genotyping remains a luxury reserved for tertiary centers. Meanwhile, peasants in flyover states are getting terbinafine prescriptions like coupons.
And you call this medicine? It’s actuarial roulette with a side of placebo.
Myson Jones
December 12, 2025 AT 06:09Just want to say thank you for posting this. I’m a 68-year-old with fatty liver and was about to start itraconazole for a persistent fungal infection. Your post made me pause. I called my doctor and we switched to micafungin. I feel like I just dodged a bullet.
Also, your point about alcohol? Yeah… I’m done with wine for now.
Rashmin Patel
December 13, 2025 AT 07:52Okay I’m so mad right now 😤 I’ve been taking terbinafine for 10 weeks and never got a single blood test - my dermatologist just said ‘it’s fine, most people are okay’ - but now I’m reading this and I’m like… why didn’t anyone tell me? I’ve been drinking coffee like a maniac and taking ibuprofen for my knees and now I’m scared to even breathe.
Also, I just found out my cousin had a liver transplant because of ketoconazole - she was 34. I’m texting everyone I know who’s on antifungals. This needs to go viral.
❤️❤️❤️
sagar bhute
December 13, 2025 AT 10:18This post is just fearmongering dressed up as medicine. Most people who get liver damage were already alcoholics or on 12 other meds. Stop scaring healthy people. I took ketoconazole for two years and my liver is fine. Your ALT numbers are meaningless without context. You’re just feeding the anxiety industrial complex.
Cindy Lopez
December 15, 2025 AT 00:01Fluconazole is the safest oral azole - correct. But only if you’re not a CYP2C19 poor metabolizer. That detail is buried in the footnote. This entire post would be stronger if it included pharmacogenomic testing as a standard recommendation, not an afterthought.
James Kerr
December 16, 2025 AT 02:23Just wanted to say thanks for posting this. I’m on itraconazole right now and was totally clueless. Just got my first blood test - all good so far. Going to keep checking weekly like you said. Also… no alcohol. Got it. 😅