Off-Label Prescribing: What It Is, Why It Happens, and What You Need to Know
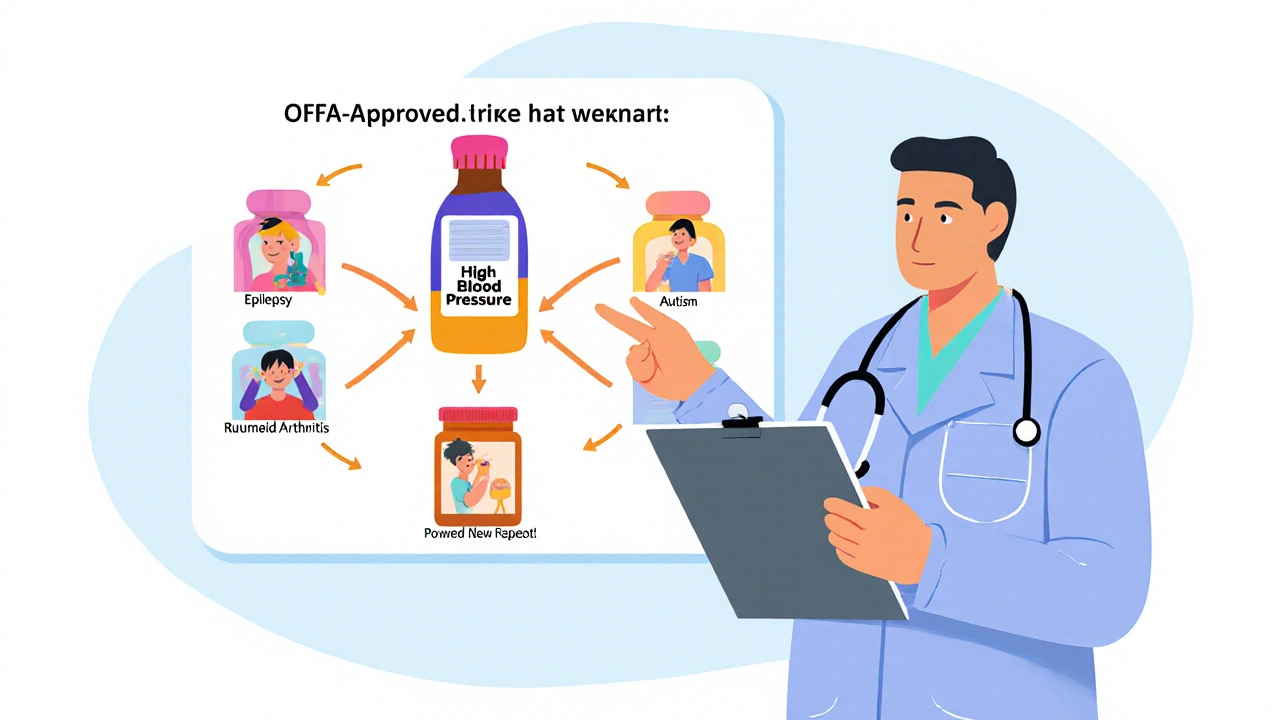
When a doctor prescribes a drug for something off-label prescribing, the use of an FDA-approved medication for a purpose not listed in its official labeling. Also known as unlabeled use, it happens every day in clinics across the country. The FDA approves drugs based on clinical trials for specific conditions—like using fluoxetine for depression. But once a drug is on the market, doctors can legally prescribe it for anything they believe will help, even if the evidence isn’t in the package insert. This isn’t a loophole—it’s a well-established part of medical practice.
Why does this happen? Sometimes, the science moves faster than the bureaucracy. A drug might show clear benefits for a new condition in real-world use, but the manufacturer never paid for the expensive trials needed to get the label updated. That’s why antidepressants, medications originally approved for depression but now commonly used for anxiety, nerve pain, or insomnia are often prescribed off-label. Same with beta-blockers, heart drugs now used to stop performance anxiety or migraine headaches. In pediatrics, it’s even more common—many drugs used in kids were never tested on them, so doctors rely on adult data and clinical judgment.
But off-label doesn’t mean unsafe. It means unapproved—for that use. The key difference is evidence. Some off-label uses are backed by strong studies and decades of clinical experience. Others? Not so much. That’s why you’ll find posts here about off-label prescribing tied to real cases: grapefruit juice boosting statin levels, compounded meds filling gaps when standard pills won’t work, or NTI drugs like warfarin where even tiny formulation changes can cause harm. These aren’t random examples—they’re warning signs that off-label use needs careful monitoring.
Patients often don’t know they’re on a drug off-label. Doctors don’t always explain it. But you have a right to ask: "Is this FDA-approved for my condition?" and "What’s the evidence for this use?" If your doctor says yes to an off-label drug, make sure they’re not just guessing. Look for peer-reviewed studies, guidelines from medical societies, or real patient outcomes. The posts below cover exactly this—how generic substitutions affect seizure control, why boxed warnings change over time, and how manufacturing defects in generics can make off-label use riskier. This isn’t about rejecting off-label use. It’s about using it wisely—knowing when it’s smart, when it’s necessary, and when you should push for more answers.
Off-label drug use is legal, common, and often necessary - especially in pediatrics, oncology, and psychiatry. Learn why doctors prescribe medications beyond FDA approval and how patients can navigate the risks and insurance hurdles.
Nov, 16 2025