Off-Label Drug Use: Why Doctors Prescribe Medications Beyond FDA Approval
Off-Label Drug Use Checker
Check Off-Label Prescription Status
Enter a drug name and condition to see if this combination is commonly prescribed off-label, the evidence level, and insurance coverage information.
Every year, millions of Americans take medications that weren’t officially approved by the FDA for their specific condition. That’s not a mistake. It’s not illegal. And in many cases, it’s the best option they have.
What Off-Label Drug Use Actually Means
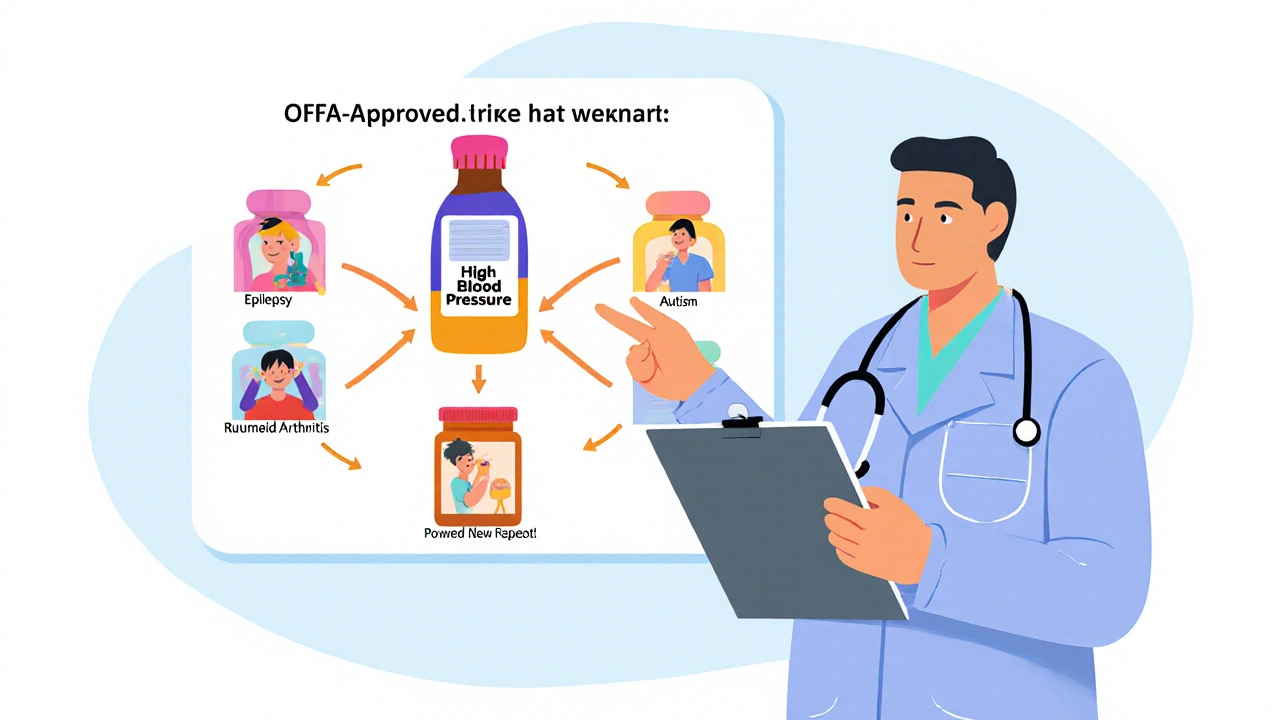
When a drug gets FDA approval, it’s cleared for a specific use - like treating high blood pressure, depression, or a certain type of cancer. That’s called the on-label use. But once that drug is on the market, doctors can legally prescribe it for anything else they believe will help a patient. That’s off-label use.
It could mean giving a drug meant for adults to a child. Or using a pill meant for oral intake as an injection. Or prescribing a cancer drug for a different tumor type than what it was tested on. The FDA doesn’t control how doctors practice medicine - only how drugs are marketed and tested before approval.
Think of it like this: The FDA says, “This drug works for Condition A.” But they don’t say, “You can’t use it for Condition B if you think it’ll help.” That’s where clinical judgment comes in.
Why Off-Label Use Is So Common
One in five prescriptions in the U.S. is off-label. That’s not rare. It’s routine. In some areas, it’s the norm.
- In pediatrics, about 62% of prescriptions are off-label because most drugs were never tested on kids.
- In psychiatry, roughly 31% of prescriptions are for uses not on the label - like using antipsychotics for insomnia or anxiety.
- In oncology, up to 85% of chemotherapy drugs are used off-label. Cancer doesn’t care about FDA labels. If a drug blocks a mutation in lung cancer, doctors will try it on breast cancer if the biology matches.
Why? Because the system moves slowly. Getting a new indication approved can cost $50-100 million and take five to seven years. Meanwhile, patients are suffering. Doctors see real-world results - a drug works for a rare autoimmune disease, or a diabetes med helps with weight loss - and they act on it.
Take methotrexate. Originally approved for cancer and psoriasis. Now it’s used for rheumatoid arthritis, Crohn’s disease, and even ectopic pregnancies. None of those uses were in the original label. But decades of evidence made it standard care.
The Legal and Ethical Boundaries
It’s legal for doctors to prescribe off-label. It’s illegal for drug companies to promote it.
Pharmaceutical companies can’t tell doctors, “This drug works for depression,” if it’s only approved for migraines. That’s considered illegal promotion. And the penalties are steep. GlaxoSmithKline paid $3 billion in 2012 for pushing off-label uses of Paxil and Wellbutrin. Pfizer paid $2.3 billion in 2012 for promoting Bextra for unapproved heart conditions.
Doctors, on the other hand, are free to use their judgment. But that freedom comes with responsibility. The American Medical Association says off-label prescribing is acceptable only when it’s based on solid science, published studies, or expert consensus.
That’s why many hospitals require doctors to document why they’re prescribing off-label - what studies they’re relying on, what alternatives were considered, and what risks the patient was told.

When Off-Label Use Saves Lives
There are countless stories where off-label use made the difference between life and death.
A 2021 case in the New England Journal of Medicine described a young woman with a rare autoimmune disorder. All FDA-approved treatments failed. Her doctors tried intravenous immunoglobulin - a drug approved for immune deficiencies, not this condition. She recovered. It took three months of insurance appeals to get coverage, but she lived.
Another example: Vincristine, a chemo drug, is often given weekly instead of every two weeks for certain rare sarcomas. Studies show better outcomes. But the label says biweekly. So doctors prescribe it off-label - and fight with insurers every time.
These aren’t experiments. They’re evidence-based decisions made by experienced clinicians who’ve seen the data, reviewed the literature, and know their patient’s history.
The Hidden Risks
But off-label use isn’t always safe.
The infamous Fen-Phen case is a warning. Fenfluramine and phentermine were prescribed together for weight loss - an off-label combo. Years later, thousands of patients developed severe heart valve damage. The drugs were pulled from the market. No one had tested this combination properly.
Today, similar concerns surround GLP-1 agonists like Ozempic and Wegovy. Originally approved for type 2 diabetes, they’re now wildly popular for weight loss. Sales have exploded. But long-term safety data for this use? Still limited. Side effects like nausea, gallbladder issues, and potential muscle loss aren’t fully understood in healthy, non-diabetic people.
And then there’s the issue of evidence quality. A 2018 study in JAMA Internal Medicine found that 78% of off-label uses had weak or no scientific backing. Only 22% were supported by strong clinical trials.
That’s why some doctors are cautious. A 2022 Medscape survey showed 67% of primary care physicians worry about liability when prescribing off-label - even though it’s legal.
Insurance and Access: The Real Barrier
Even when a drug makes sense off-label, getting it covered is a nightmare.
Insurance companies like UnitedHealthcare require off-label uses to meet strict criteria: either it’s listed in a recognized compendium like the National Comprehensive Cancer Network (NCCN), or it’s backed by peer-reviewed studies. If not? You pay out of pocket.
For cancer patients, that can mean thousands of dollars extra. A 2023 study in JAMA Network Open found that 45% of physicians reported insurance delays added 3 to 5 days to treatment start times - time patients with aggressive cancers don’t have.
And it’s not just cancer. A parent trying to get their child with a rare seizure disorder on a drug approved for adults may spend months appealing denials. The drug works. The science supports it. But the label doesn’t say so. So the insurer says no.

How Doctors Decide What’s Safe
It’s not random. Good doctors don’t just guess.
They check resources like:
- NCCN Compendium - the gold standard for cancer off-label uses
- DRUGDEX - a clinical database with evidence ratings
- PubMed - peer-reviewed studies
- Off-Patent Drugs Database - for older drugs with real-world use data
They also look at the type of evidence:
- High-quality: Systematic reviews, randomized trials
- Medium: Cohort studies, case-control studies
- Low: Case reports, expert opinion
And they talk to patients. Not just about benefits, but about unknowns. “This isn’t on the label. Here’s what we know. Here’s what we don’t. What do you want to do?”
The Future: Real-World Evidence and Faster Approvals
The FDA is starting to catch up.
The 21st Century Cures Act of 2016 let the agency use real-world data - from electronic health records, patient registries, and insurance claims - to support new drug approvals. In 2023, the FDA released draft guidance to make this easier.
Imagine this: A drug is used off-label for 10 years in thousands of patients. Data shows it’s safe and effective for a new use. Instead of waiting five years for a new trial, the FDA can review this real-world evidence and approve it faster.
That could reduce off-label use over time - not by banning it, but by making it official.
But even with faster approvals, off-label prescribing won’t disappear. Rare diseases. Pediatric needs. Cancer mutations. These will always outpace the approval process.
As FDA Commissioner Robert Califf said in 2023: “Off-label use remains a necessary component of medical practice. But we must improve mechanisms for generating evidence to support these uses more efficiently.”
Bottom Line: It’s Not About Breaking Rules - It’s About Filling Gaps
Off-label drug use isn’t a loophole. It’s a lifeline.
It’s how a child with a rare seizure disorder gets treatment. How a cancer patient with no approved options finds hope. How a veteran with PTSD gets relief when SSRIs don’t work.
But it’s also where risk lives - when evidence is thin, when insurers say no, when patients aren’t fully informed.
The goal isn’t to stop off-label use. It’s to make it smarter. Better documented. Better supported by data. And easier to access.
Because medicine isn’t about sticking to labels. It’s about helping people - even when the system hasn’t caught up yet.
Is off-label drug use legal in the U.S.?
Yes, it’s completely legal for doctors to prescribe FDA-approved drugs for uses not listed on the label. The FDA regulates drug approval and marketing, but it doesn’t control how physicians practice medicine. This has been upheld in court rulings since the 1960s.
Why don’t drug companies get more drugs approved for more uses?
Getting a new FDA approval costs $50-100 million and takes 5-7 years. For older drugs, generic manufacturers have little incentive to fund trials. For newer drugs, companies often focus on the most profitable indications first. Off-label use fills the gap while companies decide if it’s worth the investment.
Can I get insurance to cover an off-label drug?
Sometimes. Insurers like UnitedHealthcare and Medicare require off-label uses to be supported by strong evidence - usually from recognized compendia like NCCN or DRUGDEX, or published peer-reviewed studies. Without that, coverage is often denied, and patients may have to pay out of pocket or appeal the decision.
Are off-label drugs less safe than on-label ones?
Not necessarily. The same drug is the same drug. But safety data may be limited for the off-label use. For example, a drug proven safe for adults may have unknown risks in children. Or a cancer drug used for a different tumor type may have unexpected side effects. The key is whether the prescribing doctor has reviewed available evidence.
What’s the difference between off-label use and drug abuse?
Off-label use is a medical decision made by a licensed provider based on clinical evidence. Drug abuse is taking a medication without a prescription, in higher doses, or for non-medical reasons - like getting high. Off-label prescribing is legal and often life-saving. Drug abuse is dangerous and illegal.
How can I know if my doctor is prescribing off-label for good reasons?
Ask. A good doctor will explain why they’re choosing an off-label option, what evidence supports it, and what alternatives exist. They should also discuss potential risks, especially if the use is experimental. If they can’t point to studies, guidelines, or expert recommendations, it’s worth getting a second opinion.

Andrew Cairney
November 17, 2025 AT 02:34They're lying to you. The FDA doesn't care about safety - they're paid off by Big Pharma. Off-label use? That's just the loophole the corporations want you to believe is 'medical freedom.' Meanwhile, your kid's seizure med gets denied because the label says 'adults only' - but the real reason? They haven't squeezed enough profit out of it yet. Wake up. This isn't science. It's capitalism with a stethoscope. 🤡
Rob Goldstein
November 18, 2025 AT 16:56Just want to say - this is one of the most important topics in modern medicine and you nailed it. The NCCN compendium is the real MVP here. I’ve seen oncologists use off-label regimens that saved lives when standard protocols failed. The key is documentation and evidence. If you’re prescribing off-label, you better have PubMed open and a solid rationale. It’s not magic - it’s medicine at its most human.
vinod mali
November 19, 2025 AT 08:09Jennie Zhu
November 19, 2025 AT 10:58It is imperative to underscore that off-label prescribing, while legally permissible, necessitates adherence to the standard of care as delineated by the American Medical Association and corroborated by peer-reviewed literature. The absence of FDA approval for a specific indication does not absolve the clinician of the duty to ensure that such prescribing is grounded in robust clinical evidence, comprehensive patient counseling, and meticulous documentation. Liability exposure remains nontrivial in the absence of these safeguards.
Kathy Grant
November 21, 2025 AT 07:53I keep thinking about that mom in the NEJM case - three months of appeals just to save her daughter’s life. It’s not just about drugs or labels. It’s about a system that treats people like data points instead of human beings. We’re supposed to be healing people. Not fighting insurance bots. Not waiting for a bureaucracy to catch up to what a doctor sees in front of them every day. I cry every time I read stories like this. Not because it’s sad - because it’s wrong. And we’re all complicit if we don’t change it.
Robert Merril
November 22, 2025 AT 15:36Noel Molina Mattinez
November 22, 2025 AT 17:54Roberta Colombin
November 22, 2025 AT 20:05Thank you for sharing this thoughtful and balanced perspective. As someone who works with families navigating rare conditions, I see how off-label prescribing becomes a bridge when no other path exists. It is not about bending rules - it is about honoring dignity, hope, and the quiet courage of clinicians who choose to act when systems fail. We must support them with better data, not blame them for trying.
Dave Feland
November 22, 2025 AT 21:02Let’s be intellectually honest: Off-label prescribing is a symptom of systemic regulatory failure. The FDA’s approval process is a charade designed to appease public sentiment while enabling pharmaceutical monopolies. The real scandal isn’t doctors prescribing off-label - it’s that the system incentivizes drug companies to delay evidence generation until patent expiration. This isn’t medical innovation - it’s legal arbitrage. And anyone who calls this ‘lifeline’ is either naive or complicit.