Generic Substitution: What It Is, When It Works, and When to Say No
When your pharmacist hands you a different pill than what your doctor prescribed, that’s generic substitution, the practice of swapping a brand-name drug for a chemically identical generic version at the pharmacy level. Also known as automatic substitution, it’s legal in most places and meant to cut costs—but it’s not risk-free.
Not all drugs are created equal when it comes to substitution. Narrow therapeutic index (NTI) drugs, medications where tiny changes in dosage can cause serious harm or treatment failure like warfarin, levothyroxine, and phenytoin are especially tricky. Even a 5% difference in absorption can turn a stable patient into someone in the ER. That’s why 27 U.S. states, have laws that block automatic generic substitution for these critical drugs. In those places, your pharmacist must get your doctor’s OK before switching. Other states? They let the pharmacist decide unless you say no.
It’s not just about laws. Manufacturing defects, like uneven dosing, tablet capping, or contamination in generic production happen more often than most people realize. One batch might work perfectly; the next might cause side effects because of a slight change in fillers or coating. That’s why some patients stick with brand names—even if it costs more—because their body reacts predictably to the same formula. And if you’re on a drug where timing matters—like seizure meds or heart rhythm drugs—even a small delay in absorption can throw off your whole treatment.
Generic substitution isn’t good or bad—it’s situational. For antibiotics, blood pressure meds, or antidepressants, it’s often perfectly safe and saves hundreds a year. But for drugs where precision is life-or-death, skipping the brand could mean skipping your next doctor visit. The key? Know your meds. Ask your pharmacist: "Is this a generic?" and "Is it safe to switch?" If you feel different after the switch—dizzy, tired, or out of control—don’t ignore it. Track your symptoms. Talk to your doctor. And if you’re on a critical medication, consider asking for a "Do Not Substitute" note on your prescription. You’re not being difficult—you’re being smart.
Below, you’ll find real patient stories, state-by-state rules on NTI drugs, and comparisons of generic failures that changed lives. These aren’t theoretical debates—they’re cases where someone’s health hung in the balance because substitution wasn’t handled right. Whether you’re switching meds yourself or helping a loved one, this collection gives you the facts to protect yourself.
Learn how to talk to your pharmacy during generic drug transitions to avoid side effects, ensure effectiveness, and save money. Most generics are just as good as brands - but communication makes all the difference.
Feb, 15 2026
Switching to generic respiratory inhalers can save money-but only if done right. Learn why the device matters more than the drug, how improper use leads to worse symptoms, and what steps to take before swapping your inhaler.
Dec, 15 2025
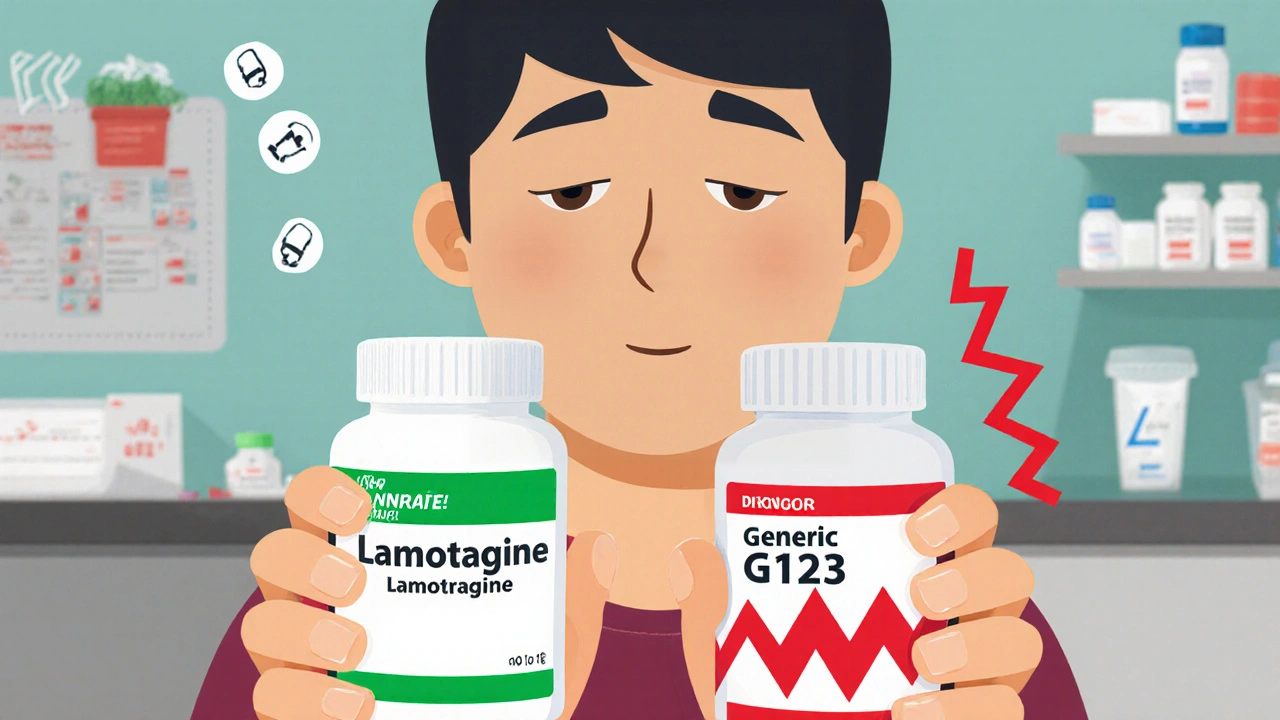
Generic antiseizure medications can save money, but for narrow therapeutic index drugs like lamotrigine and carbamazepine, even small changes in formulation can trigger seizures. Learn the risks, who's most vulnerable, and how to protect yourself.
Nov, 17 2025