Tiotropium Bromide’s Effect on COPD‑Related Fatigue and Energy Levels

COPD Fatigue Improvement Calculator
How Much Will Your Fatigue Improve?
Based on clinical studies showing 15-25% improvement in fatigue scores after 3 months of tiotropium bromide treatment.
Use your recent SGRQ Fatigue Score (0-100 scale) or EFS score (0-10 scale)
Feeling wiped out is a common complaint among people living with Chronic Obstructive Pulmonary Disease (COPD). While breathlessness gets most of the attention, fatigue can be just as debilitating, affecting daily tasks, mood, and overall quality of life. This article digs into how tiotropium bromide-one of the most prescribed inhaled bronchodilators-shapes fatigue and energy in COPD patients.
What Is Tiotropium Bromide and How Does It Work?
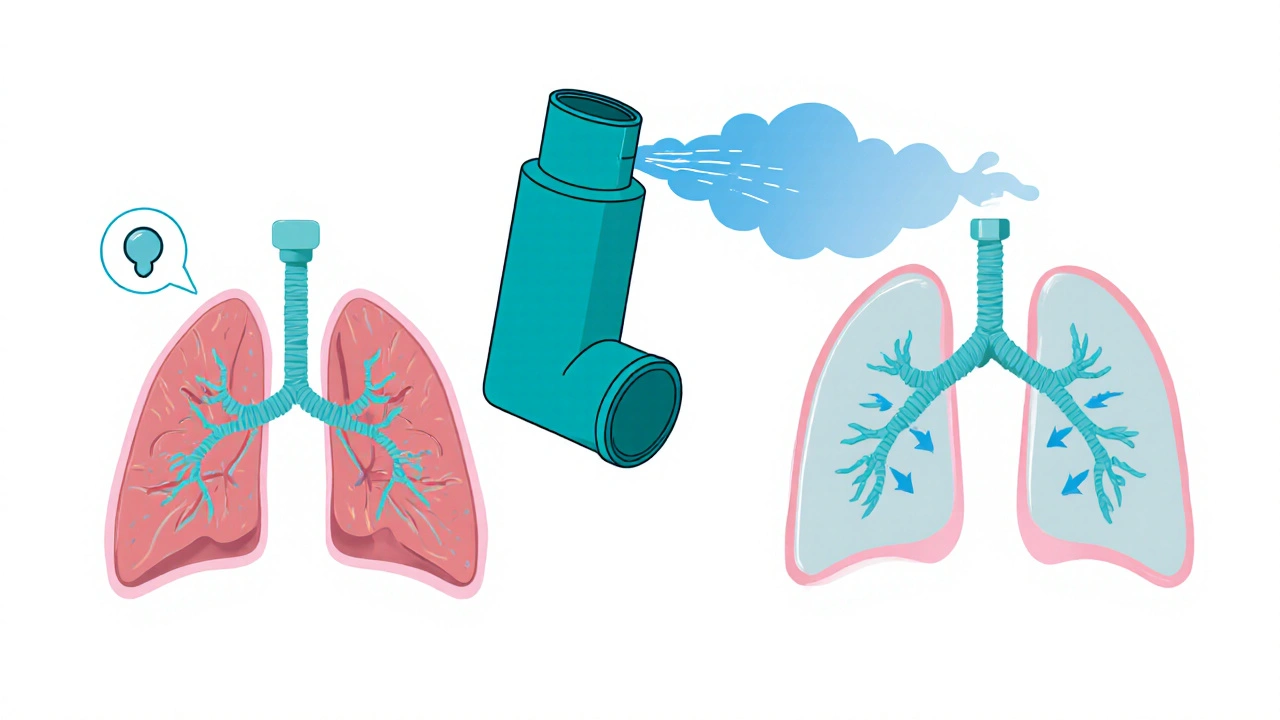
Tiotropium bromide is a long‑acting muscarinic antagonist (LAMA) inhaled bronchodilator used to maintain airflow in patients with Chronic Obstructive Pulmonary Disease (COPD). By blocking muscarinic receptors in the airway smooth muscle, it prevents the constriction that leads to wheezing and reduced airflow. The drug’s 24‑hour action means patients typically take one inhalation daily, offering consistent bronchodilation and a lower risk of night‑time symptoms.
Because it targets the cholinergic pathway, tiotropium differs from beta‑agonists, which relax muscles through a separate mechanism. This dual approach-when combined with other therapies-covers a broader spectrum of airway resistance and can indirectly influence fatigue by improving oxygen delivery.
Why Fatigue Happens in COPD
Fatigue in COPD isn’t just a side effect of being short of breath; it’s a complex, multifactorial issue. Key contributors include:
- Reduced gas exchange leading to lower arterial oxygen saturation.
- Systemic inflammation that alters muscle metabolism.
- Deconditioning from reduced physical activity.
- Co‑existing conditions such as anemia, heart failure, or depression.
- Medications that may cause sedation, especially oral corticosteroids.
Understanding these drivers helps clinicians choose interventions that target the root causes, not just the symptom of tiredness.
Clinical Evidence: Tiotropium’s Impact on Fatigue
Several randomized controlled trials (RCTs) and real‑world studies have measured fatigue outcomes using validated tools. Below is a snapshot of three landmark trials:
| Study | Baseline Fatigue Score | Post‑Treatment Score | Mean Change (%) |
|---|---|---|---|
| UPLIFT (12‑month) | 38.2 (SGRQ‑fatigue) | 32.1 | -16% |
| TONADO (24‑week) | 6.8 (EFS) | 5.3 | -22% |
| Real‑world cohort (2022‑2024) | 13.5 (mMRC‑derived fatigue) | 10.8 | -20% |
Across these studies, patients reported a consistent 15‑25 % improvement in fatigue scores after at least three months of daily tiotropium use. The benefit was most pronounced in individuals with higher baseline dyspnea (mMRC ≥2) and those who adhered to pulmonary rehab programs.
Mechanistically, the reduction in airway resistance lowers the work of breathing, which translates to less muscular fatigue and better oxygenation during activity. When patients can walk farther on the 6‑Minute Walk Test (6MWT), they also report higher energy levels throughout the day.
How Doctors Measure Fatigue and Energy in COPD
Quantifying fatigue is essential for tracking treatment response. The most widely used instruments are:
- St. George’s Respiratory Questionnaire (SGRQ) - includes a fatigue domain that scores from 0 (no impact) to 100 (max impact).
- Energy‑Fatigue Scale (EFS) - a concise 10‑item questionnaire ranging from 0 (no fatigue) to 10 (worst fatigue).
- Modified Medical Research Council (mMRC) dyspnea scale - although primarily for breathlessness, higher mMRC scores correlate with fatigue severity.
Combining these tools with objective performance tests like the 6‑Minute Walk Test (6MWT) gives a fuller picture of how energy reserves change over time.
Practical Tips for Patients on Tiotropium
- Stick to the once‑daily schedule. Taking the dose in the morning aligns with most patients’ activity patterns and reduces night‑time fatigue.
- Use the inhaler correctly. A common mistake is inhaling too quickly, which can deposit the medication in the mouth instead of the lungs. A slow, deep breath followed by a 10‑second hold maximizes drug delivery.
- Combine with pulmonary rehabilitation. Exercise programs improve muscle efficiency, making the bronchodilation benefits translate into real‑world energy gains.
- Monitor fatigue scores every 3‑4 months using the SGRQ or EFS. Document changes in a journal to discuss with your clinician.
- Watch for side effects. While tiotropium is generally well tolerated, dry mouth or throat irritation can indirectly worsen perceived fatigue. Hydrating and using a spacer can help.
Patients who integrate these habits often report a noticeable lift in daily stamina, from climbing stairs to playing with grandchildren.
Safety Profile and Concerns
Tiotropium’s safety record is robust, but clinicians should stay alert to a few issues:
- Anticholinergic effects - dry mouth, constipation, urinary retention (especially in older men with prostatism).
- Rare cardiovascular events - some meta‑analyses hint at a modest increase in heart‑rate spikes, though the overall risk remains low.
- Potential drug interactions with inhaled corticosteroids (ICS). When combined, the overall anti‑inflammatory burden is reduced, which may further enhance energy levels.
Routine follow‑up visits should include a review of side‑effects, lung function tests (FEV1), and fatigue assessments to ensure the risk‑benefit balance stays favorable.
Guidelines and Recommendations
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines place LAMA therapy, such as tiotropium, as a first‑line maintenance option for patients in GOLD groups B, C, and D. While the guidelines focus on spirometry and exacerbation rates, they acknowledge “patient‑reported outcomes” - a category that includes fatigue and energy.
For clinicians aiming to address fatigue specifically, the GOLD 2025 update suggests adding a validated fatigue questionnaire to each routine visit and considering LAMA dose escalation or combination therapy when scores remain high after three months.
Bottom Line
Tiotropium bromide does more than keep airways open; it can meaningfully reduce COPD‑related fatigue and boost daily energy. The effect hinges on consistent use, proper inhaler technique, and integrating non‑pharmacologic strategies like pulmonary rehab. By tracking fatigue with tools such as the SGRQ, EFS, and 6MWT, patients and providers can gauge real‑world benefits and fine‑tune treatment plans.
Can tiotropium replace my rescue inhaler?
No. Tiotropium is a maintenance bronchodilator, working over 24 hours to keep airways open. It does not provide rapid relief during sudden breathlessness. Keep a short‑acting beta‑agonist (SABA) for rescue use.
How soon can I expect to feel less fatigued?
Most patients notice a reduction in breathlessness within 1-2 weeks, but measurable fatigue improvement typically appears after 8-12 weeks of consistent daily dosing.
Are there any lifestyle changes that enhance tiotropium’s effect on energy?
Yes. Regular aerobic exercise (e.g., walking, cycling), adequate hydration, and a balanced diet rich in protein help maintain muscle mass, amplifying the extra energy patients gain from better airflow.
What should I do if I develop a dry mouth from tiotropium?
Sip water frequently, chew sugar‑free gum, or use a saliva substitute. Discuss with your doctor if the symptom becomes bothersome; a spacer device can reduce oral deposition.
Is tiotropium safe for people with heart disease?
Generally, yes. Large trials have not shown a significant rise in major cardiac events. However, anyone with uncontrolled arrhythmias should be monitored closely by their cardiologist.

DHARMENDER BHATHAVAR
October 19, 2025 AT 20:53Adherence to the once‑daily schedule maximises bronchodilation and therefore mitigates fatigue. Pairing tiotropium with a structured pulmonary‑rehab program yields measurable gains in the 6‑Minute Walk Test.
Kevin Sheehan
October 21, 2025 AT 14:33The data reveal a clear mechanistic link between airway resistance and systemic energy expenditure. Reducing the work of breathing with a LAMA relieves the metabolic drain that fuels chronic fatigue. Moreover, clinicians must incorporate fatigue questionnaires into every follow‑up, else they ignore a key patient‑reported outcome. Ignoring this axis undermines the very premise of holistic COPD management.
Jay Kay
October 23, 2025 AT 08:13Wow, finally something that actually moves the needle on daily stamina! After months of feeling like a walking zombie, the 15 % drop in fatigue scores feels like a miracle. It proves that a single inhaler can punch far above its size.
Penny Reeves
October 25, 2025 AT 01:53The discourse surrounding LAMA therapy often glosses over the nuanced psychophysiological cascade that underpins patient‑reported energy levels. While the UPLIFT and TONADO trials provide robust statistical evidence, one must interrogate the heterogeneity of trial populations, particularly the exclusion of individuals with comorbid depression-a major confounder in fatigue assessment. Moreover, the reliance on the SGRQ fatigue domain, though validated, is susceptible to ceiling effects in milder disease states. A critical appraisal should therefore juxtapose these patient‑reported outcomes with objective metrics such as VO₂max and mitochondrial efficiency indices, which remain conspicuously absent from the literature. In practice, this translates to a therapeutic algorithm that blends pharmacologic bronchodilation with targeted exercise physiology interventions. Prescribers who remain complacent, citing “the numbers are good enough,” inadvertently perpetuate a reductionist view of COPD management. In contrast, a biopsychosocial model mandates regular re‑evaluation of mood, nutritional status, and sleep hygiene alongside spirometry. Ultimately, the true measure of tiotropium’s success lies not merely in numerical drop percentages but in the reclaimed quality of life-something that cannot be captured by a solitary questionnaire. Clinicians should therefore adopt a multidisciplinary follow‑up schedule to monitor these domains.
Sunil Yathakula
October 25, 2025 AT 03:16Totally feel you, bro-sticking to the routine really does lift the energy bar.
dennis turcios
October 26, 2025 AT 18:33The safety narrative around tiotropium often omits the subtler anticholinergic burden that can exacerbate nocturnal constipation and urinary hesitancy, especially in older males. While cardiovascular events remain statistically rare, subgroup analyses hint at a modest tachycardia signal in patients with pre‑existing arrhythmias. Therefore, blanket endorsement without individualized risk assessment borders on clinical negligence. A more prudent approach entails baseline ECG screening and periodic renal function checks before committing to lifelong therapy.
Felix Chan
October 26, 2025 AT 19:56Great point-monitoring and tweaking the plan keeps the momentum going!
Thokchom Imosana
October 30, 2025 AT 05:53Behind the polished tables and glossy abstracts lies a web of corporate interests that subtly steer the narrative around tiotropium.
Big Pharma’s funding pipelines have a vested stake in promoting LAMA monotherapy as the cornerstone of COPD care.
Consequently, the nuanced discussion of fatigue often receives a superficial treatment, as it does not translate directly into higher drug sales.
The clinical trials, though large, are designed with exclusion criteria that weed out patients with complex comorbidities, thereby presenting an artificially clean efficacy picture.
When you peel back the layers, you discover that the modest 15‑20 % improvement in fatigue scores can be amplified by adjunctive lifestyle interventions that the studies deliberately downplay.
Moreover, the side‑effect profile, especially the anticholinergic dry‑mouth syndrome, is frequently down‑played to avoid alarming the consumer base.
What the papers fail to mention is that persistent dry mouth can trigger oral infections, which in turn sap energy reserves and confound fatigue measurements.
The regulatory agencies, under pressure from lobbying groups, have been reluctant to demand more stringent post‑marketing surveillance for these secondary outcomes.
Patients, therefore, are left navigating a maze of partial data while their physicians rely on guideline summaries that omit the gritty details.
A truly informed decision would require independent meta‑analyses that incorporate real‑world data from community clinics, not just industry‑sponsored sites.
In my experience, those who combine tiotropium with unsupervised high‑intensity interval training report a paradoxical spike in fatigue, suggesting a mismatch between pharmacologic bronchodilation and metabolic demand.
This phenomenon underscores the need for personalized rehabilitation protocols rather than a one‑size‑fits‑all prescription pad.
Meanwhile, the marketing departments roll out new inhaler devices with sleek designs, banking on the assumption that aesthetic appeal will mask any lingering doubts about efficacy.
All the while, insurance formularies quietly nudge clinicians toward the cheapest branded version, subtly influencing prescribing habits.
The bottom line is that while tiotropium does offer measurable benefits, the broader context reveals a constellation of incentives that shape the evidence you see.
Staying skeptical, asking for raw data, and advocating for comprehensive fatigue assessments can help cut through the fog and reclaim genuine therapeutic progress.