Therapeutic Drug Monitoring for Generic NTIs: Protecting Patients on Critical Antiretroviral Therapies
When a patient switches from a brand-name antiretroviral drug to a generic version, they’re often told it’s the same thing-chemically identical, just cheaper. But for drugs with a narrow therapeutic index, that assumption can be dangerous. Therapeutic Drug Monitoring (TDM) isn’t a luxury for these cases-it’s a safety net. For patients on generic versions of drugs like lopinavir, ritonavir, or dolutegravir, even small differences in absorption or metabolism can push drug levels below the threshold needed to suppress HIV-or high enough to cause liver damage, nerve toxicity, or severe rashes.
Why TDM Matters for Generic NTIs
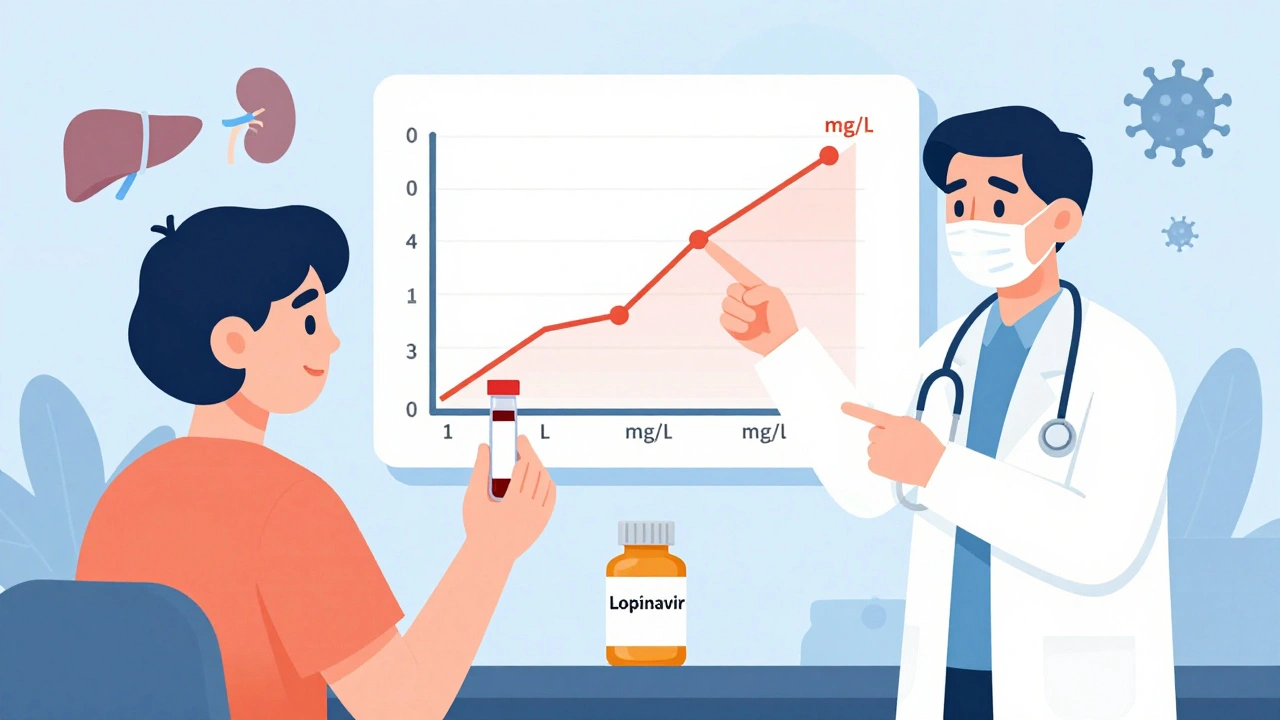
Not all antiretroviral drugs are created equal when it comes to how they behave in the body. Drugs with a narrow therapeutic index (NTI) have a tiny gap between the dose that works and the dose that harms. A 10% drop in concentration might mean the virus starts replicating. A 15% rise could mean toxic side effects. This is especially true for protease inhibitors (PIs) and non-nucleoside reverse transcriptase inhibitors (NNRTIs), which are commonly used in first-line and salvage regimens. Generic versions of these drugs must meet bioequivalence standards-but those standards are based on average performance across healthy volunteers. Real patients? They have different gut pH, liver function, kidney clearance, and drug interactions. A patient with HIV and tuberculosis on rifampin? That drug can slash PI levels by 40%. A patient with chronic diarrhea from long-term ART? Absorption drops. An elderly patient on multiple medications? Drug interactions pile up. In these cases, assuming bioequivalence equals therapeutic equivalence is a gamble with someone’s life.How TDM Works-And What It Can’t Do
TDM measures the concentration of a drug in a patient’s blood plasma, usually at the lowest point before the next dose (called the trough level). For drugs like lopinavir, the target range is typically 1-4 mg/L. If it’s below 1, the virus may develop resistance. If it’s above 4, liver toxicity becomes likely. The test itself is simple: a blood draw, sent to a specialized lab with validated assays. Results come back in 10-14 days in public health systems, or as fast as 48 hours in private labs. But TDM doesn’t work for everything. It’s useless for NRTIs like tenofovir or emtricitabine. Why? Because those drugs are prodrugs-they need to be activated inside cells. What matters isn’t the blood level, but the concentration of the active form inside white blood cells. That’s not measurable with standard TDM. So if your patient is on a regimen like Truvada + dolutegravir, TDM only helps with the dolutegravir part. The NRTI component? You monitor viral load instead.When TDM Makes the Biggest Difference
TDM isn’t for everyone. But in these five situations, it can be life-changing:- Switching to a generic PI or NNRTI-Especially if the patient has a history of treatment failure or side effects.
- Drug interactions-Like rifampin for TB, or certain antifungals or seizure meds that alter liver enzyme activity.
- Poor absorption-Patients with Crohn’s, celiac disease, or chronic diarrhea.
- Renal or liver impairment-Dosing guidelines aren’t precise enough for advanced organ damage.
- Pediatric or elderly patients-Metabolism changes dramatically with age or growth.
The Hidden Costs and Barriers
TDM isn’t cheap. In the UK, each test costs £250-£350. In the U.S., private labs charge $450-$650. Insurance rarely covers it unless there’s a documented reason. Many clinics don’t offer it because they don’t have a lab partner. Turnaround time is another problem. Waiting two weeks for results means you might miss the window to prevent treatment failure. By the time the lab report arrives, the patient’s viral load may have already spiked. And interpreting the results? That’s not something a general practitioner can do. It requires training in pharmacokinetics, familiarity with HIV drug interactions, and access to reference ranges specific to each drug and assay. The European Association of Clinical Microbiology and Infectious Diseases says clinicians need 6-12 months of mentorship before they can reliably use TDM.What the Guidelines Say
The U.S. Department of Health and Human Services doesn’t recommend routine TDM for HIV. The European AIDS Clinical Society (EACS) says it’s only for specific cases. The UK HIV guidelines are more practical: they list clear indications-drug interactions, poor absorption, organ damage, pediatric dosing. That’s the sweet spot. The controversy isn’t whether TDM works-it’s whether it’s worth the cost and complexity for most patients. Studies show TDM reduces treatment failure by 15-20% in complex cases. One 2022 pilot in South Africa found a 22% drop in treatment failure among patients on generic antiretrovirals who received TDM-guided dosing. But those are specialized settings. In a busy clinic in rural Kansas? It’s not feasible.How to Use TDM Wisely
If you’re managing a patient on a generic NTI drug, here’s how to approach TDM without overcomplicating things:- Don’t test routinely. Only use it when one of the five high-risk situations applies.
- Pair it with viral load testing. TDM tells you about drug levels. Viral load tells you if the virus is still being suppressed. Use both.
- Know your lab’s turnaround time. If it’s longer than 10 days, consider a private lab for urgent cases.
- Don’t use TDM to replace adherence counseling. A patient skipping doses won’t benefit from a dose increase-they need support, not more pills.
- Work with a specialist. Infectious disease pharmacists or HIV specialists can interpret results and adjust doses safely.
The Future of TDM
Newer drugs like dolutegravir and bictegravir are more forgiving, with wider therapeutic windows. But as more patients are treated with generic versions globally-especially in low-resource countries-TDM is becoming a tool for equity. In South Africa, pilot programs use TDM to ensure generic antiretrovirals aren’t failing because of poor absorption or substandard formulations. In Canada, McGill University Health Centre has expanded TDM services to include newer integrase inhibitors when used with TB drugs. The real win isn’t just better dosing-it’s preventing resistance. When a patient fails on a generic drug because levels were too low, they may develop resistance to the entire class. That limits future options. TDM helps avoid that domino effect.What Patients Should Know
If you’re on a generic antiretroviral and your provider suggests TDM, ask: Why now? Is it because of a new drug, a change in health, or side effects? Don’t assume it’s standard. But also don’t refuse it if you’re in a high-risk group. This isn’t about money-it’s about making sure the medicine you’re taking actually works the way it should.Frequently Asked Questions
Is therapeutic drug monitoring the same as viral load testing?
No. Viral load testing measures how much HIV is in your blood-whether the virus is being suppressed. TDM measures how much of the drug is in your bloodstream. One tells you if the treatment is working; the other tells you if you’re getting the right amount of drug. You need both in complex cases.
Can TDM be used for all HIV medications?
No. TDM works for protease inhibitors (like lopinavir) and non-nucleoside reverse transcriptase inhibitors (like efavirenz). It does not work for NRTIs (like tenofovir or emtricitabine) because these drugs need to be activated inside cells, not measured in blood. TDM also isn’t useful for newer entry inhibitors or attachment inhibitors.
Why do some clinics refuse to do TDM?
Cost and logistics. TDM requires specialized labs, trained staff, and time to interpret results. Many clinics don’t have access to reference labs that offer HIV-specific TDM. Insurance often won’t cover it unless there’s a clear clinical reason. In some places, it’s simply not available.
How long does it take to get TDM results?
In public health systems, results typically take 10-14 days. Private labs can deliver them in 2-3 days, but they cost $450-$650 per test. Delays are a major drawback-by the time results come back, a patient may have already developed resistance or toxicity.
Is TDM worth it for generic drugs?
Yes-if you’re in a high-risk group. For patients with kidney or liver disease, drug interactions, poor absorption, or pediatric dosing, TDM can prevent treatment failure and toxicity. For healthy patients on stable regimens without interactions, it’s usually unnecessary. The value is in targeted use, not routine screening.

Jade Hovet
December 10, 2025 AT 23:25OMG this is SO important!!! 🙌 I know someone on generics who started getting crazy liver issues and no one knew why until they did TDM-turns out the generic was absorbing like garbage. Why aren’t we doing this for everyone?!?! 😭
nithin Kuntumadugu
December 12, 2025 AT 18:52Lmao sure, let’s spend $600 per test so Big Pharma can keep pretending generics are ‘safe’. 😏 Meanwhile, the real problem? The FDA lets these companies tweak bioequivalence thresholds like they’re playing Monopoly. You think the lab results are accurate? Nah. They’re just another corporate loophole. 🤡
John Fred
December 13, 2025 AT 22:02Really appreciate this breakdown-especially the part about NRTIs not being measurable via TDM. Pharmacokinetics is wild, man. For PIs and NNRTIs, TDM is a game-changer when you’ve got polypharmacy or GI issues. Just don’t forget to correlate with viral load. A low drug level + detectable VL = red flag. 🚩
Harriet Wollaston
December 14, 2025 AT 17:11This hit me right in the heart. I’ve seen patients cry because they were told ‘it’s the same pill’-but then they got sick. No one told them it might not be. TDM isn’t fancy-it’s just fair. Everyone deserves to know their medicine is working, not just the people who can afford private labs. 💛
Lauren Scrima
December 16, 2025 AT 16:03So… we’re spending $350 to find out what adherence counseling should’ve told us? 🤔 I mean, if your patient’s skipping doses, TDM won’t fix that-it’ll just give you a fancy number to blame the generic for. And who’s gonna pay for the 6-month mentorship? 😅
sharon soila
December 17, 2025 AT 23:42Every human being deserves to live without fear that their medicine is broken. This is not about cost. This is about dignity. If a pill can save a life-or end it-then we must know, with certainty, that it is working. TDM is not a luxury. It is a moral obligation. Let us not wait for a tragedy to act. The science is here. The will must follow.