Parkinson's Disease Medication: What Works, What to Avoid, and How to Stay in Control
When you’re living with Parkinson's disease, a progressive nervous system disorder that affects movement, often starting with tremors and stiffness. Also known as Parkinson’s, it doesn’t just shake your hands—it can make walking, talking, and even swallowing harder over time. The right Parkinson's disease medication doesn’t cure it, but it can give you back hours of control every day. For many, that’s everything.
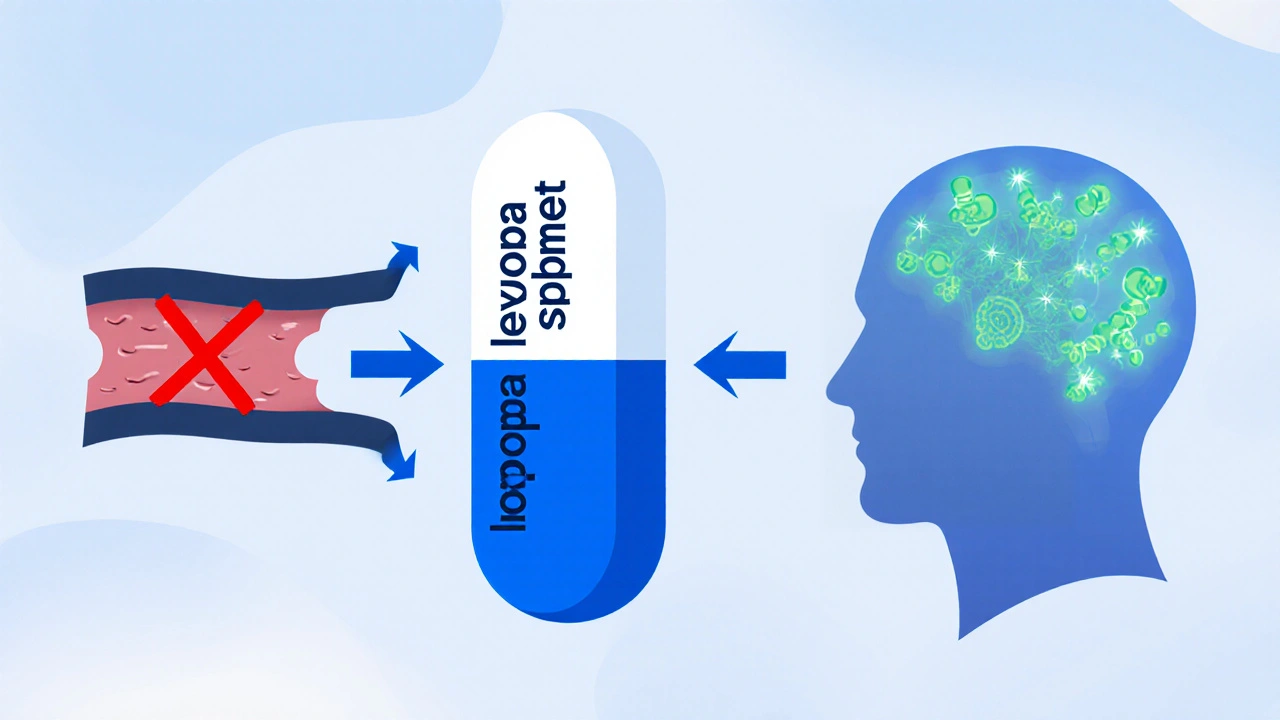
Most treatment starts with levodopa, the gold-standard drug that your brain converts into dopamine, the chemical your nerve cells stop making. It’s powerful, but it doesn’t last forever. Over time, the effects wear off faster, and you might get sudden switches between "on" and "off" states. That’s why doctors often add dopamine agonists, like pramipexole or ropinirole, which trick your brain into thinking it’s getting dopamine without actually making it. These can delay levodopa use early on, but they come with their own risks—impulse control issues, drowsiness, even hallucinations in older adults.
Then there are MAO-B inhibitors, such as selegiline and rasagiline, which slow down the breakdown of dopamine already in your system. They’re mild, often used as add-ons, and some studies suggest they might even slow progression slightly. You’ll also see COMT inhibitors, like entacapone, which help levodopa stick around longer in your blood. These aren’t stand-alone drugs—they’re partners to levodopa, meant to smooth out the highs and lows.
But here’s what no one tells you: Parkinson’s meds don’t play nice with other drugs. Antidepressants, antinausea pills, even some cold medicines can cancel out your Parkinson’s treatment or make symptoms worse. And if you’re taking supplements like coenzyme Q10 or vitamin E—common for people with Parkinson’s—some might interfere with absorption. It’s not just about picking the right pill. It’s about building a whole system that works without clashing.
Side effects aren’t just annoying—they can be dangerous. Dizziness from low blood pressure, sudden sleep attacks, swelling in the legs, or uncontrolled movements called dyskinesia. You can’t just power through them. Tracking what you take, when you take it, and how you feel each day helps your doctor adjust things before things get out of hand.
There’s no one-size-fits-all plan. What works for a 62-year-old with mild tremors might overload a 78-year-old with balance issues. That’s why the posts below dig into real comparisons: which meds are safest for older adults, how to handle nausea from levodopa, why some people need to avoid dopamine agonists entirely, and what alternatives exist when standard drugs stop working. You’ll find practical advice on timing doses around meals, managing interactions with common supplements, and spotting red flags before they become emergencies.
A detailed comparison of Sinemet with other Parkinson's disease drugs, covering mechanisms, side effects, dosing, costs, and how to choose the right therapy.
Oct, 20 2025