Switching Antidepressants: How to Reduce Side Effects During Transition
Why People Switch Antidepressants
Many people start an antidepressant hoping it will lift their mood, improve sleep, and take away the weight of depression. But for a lot of them, it doesn’t work the way it should. About 30% to 50% of people don’t get enough relief from their first try, according to data from the STAR*D trial. Others feel fine emotionally but are hit with side effects that make life harder-sexual problems, weight gain, dizziness, or nausea. These aren’t minor inconveniences. They can make someone quit their medication altogether, which often leads to a return of depression symptoms.
That’s why switching antidepressants is so common. It’s not a failure. It’s a normal part of treatment. If one drug isn’t working or is causing too much discomfort, switching to another is a smart, evidence-backed move. But doing it wrong can make things worse. Jumping from one pill to another without a plan can trigger withdrawal symptoms, anxiety spikes, or even serotonin syndrome-a rare but dangerous condition caused by too much serotonin in the brain.
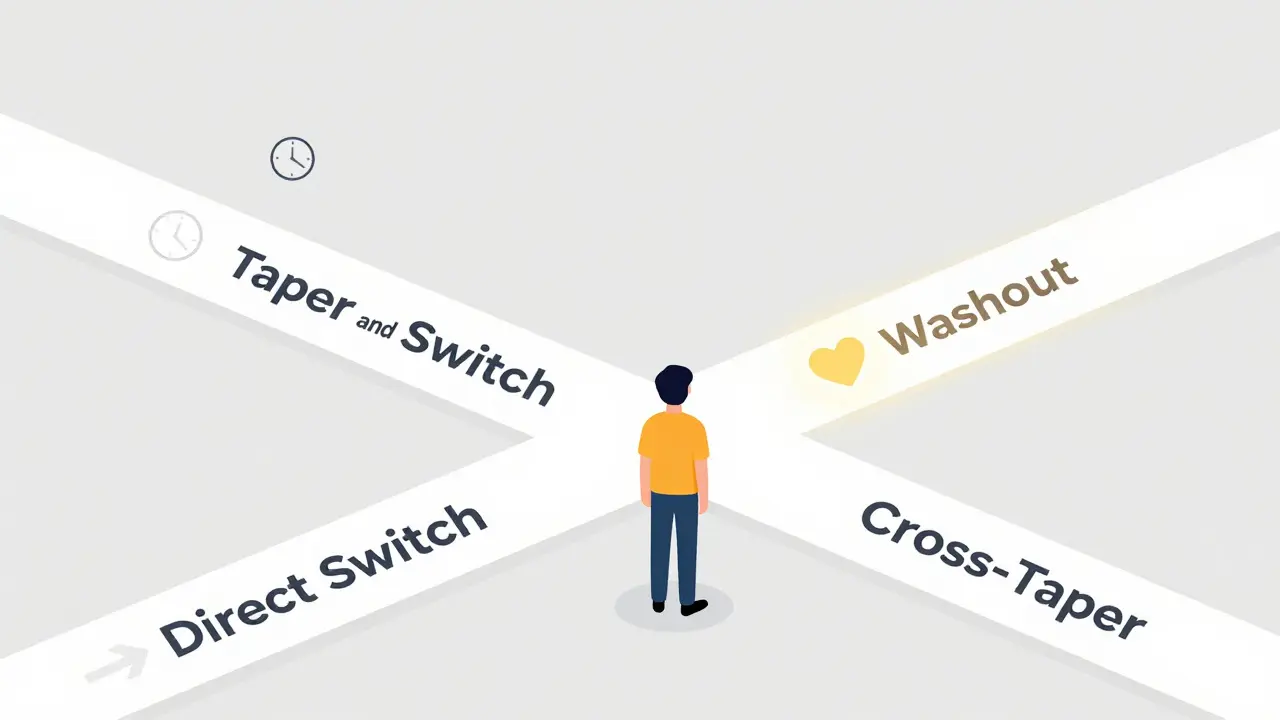
The Four Ways to Switch
There are four main ways doctors guide patients through switching antidepressants, and each has its own risks and benefits. The right one depends on the medications involved, how long you’ve been on them, and your body’s response.
- Direct switch: Stop the old drug one day and start the new one the next. This works best when moving between drugs with similar effects, like switching from one SSRI to another. But it’s risky if the old drug has a short half-life-meaning it leaves your system fast. Paroxetine and venlafaxine are examples. Stopping these suddenly can cause dizziness, brain zaps, or nausea within 24 hours.
- Taper and switch: Slowly reduce the old medication over 1-2 weeks, then stop it completely. Wait a day, then start the new one. This avoids the worst of withdrawal but leaves a gap where you’re not getting any antidepressant effect. That can trigger a relapse, especially if you’ve been on the drug for more than 8 weeks.
- Taper and switch with washout: Similar to the above, but you wait longer-sometimes 2 to 5 weeks-before starting the new drug. This is required when switching from an MAOI (like phenelzine) to any other antidepressant. It’s also needed if you’re coming off fluoxetine, which sticks around in your system for weeks because of its long half-life and active metabolites.
- Cross-taper: This is the most commonly recommended method. You slowly reduce the old medication while slowly increasing the new one at the same time. The overlap lasts 1-2 weeks. This keeps your brain chemistry more stable and cuts withdrawal symptoms by about 42%, according to a 2021 meta-analysis. It’s especially useful when switching between SSRIs or SNRIs.
For most people, cross-tapering is the safest bet. But if you’re switching from fluoxetine to an MAOI, you need that 5-week washout. No shortcuts.
Which Antidepressants Are Trickiest to Switch?
Not all antidepressants are created equal when it comes to switching. Some are like slow-moving trains-you can stop them gently. Others are like sprinters that stop on a dime and leave you stumbling.
Paroxetine and venlafaxine are the worst offenders. They have short half-lives, meaning they clear from your body quickly. If you skip a dose or cut back too fast, withdrawal hits hard. People report electric shock sensations in the head-called “brain zaps”-up to 47% of the time when switching off paroxetine. Venlafaxine switchers often get rebound anxiety and insomnia.
Fluoxetine is the opposite. It’s like a drug that lingers. Its half-life is 4-6 days, and its active metabolite can stick around for up to 15 days. That means withdrawal symptoms might not show up for weeks. But that also means it can interfere with other drugs. If you’re switching from fluoxetine to a tricyclic antidepressant like amitriptyline, you need to wait at least 5 weeks. Fluoxetine blocks the liver enzyme that breaks down tricyclics, and if you start the new drug too soon, you could build up toxic levels in your blood-leading to heart rhythm problems.
Vortioxetine and duloxetine are also tricky. They affect multiple serotonin receptors, so they can interact unpredictably with other antidepressants. Agomelatine, on the other hand, is simpler-it only really clashes with fluvoxamine.
What Withdrawal Symptoms Look Like (And How to Tell Them From Relapse)
When you stop an antidepressant, your body reacts. But that reaction isn’t the same as depression coming back.
Withdrawal symptoms show up fast-usually within 1 to 7 days of cutting your dose. Common signs include:
- Dizziness (28% of cases)
- Nausea (24%)
- Headaches (22%)
- Insomnia (19%)
- Fatigue (18%)
- “Brain zaps” (33% with paroxetine)
These aren’t just “feeling off.” They’re physical, specific, and short-lived. If you take your old medication again-even just one dose-these symptoms usually vanish within hours. That’s a clear sign it’s withdrawal, not relapse.
Relapse of depression, on the other hand, creeps in slowly. It takes weeks. You feel hopeless, lose interest in things you used to enjoy, sleep too much or too little, and have trouble concentrating. It doesn’t come with brain zaps or sudden nausea. If you’re unsure, talk to your doctor. A quick re-start of your old medication can help confirm the cause.

How to Reduce Side Effects During the Switch
There are practical steps you can take to make the transition smoother.
- Take your meds with food. This cuts nausea and stomach upset by about 35%, according to Mayo Clinic data.
- Eat smaller, more frequent meals. Large meals can make nausea worse.
- Suck on sugarless hard candy. Helps with dry mouth and nausea.
- Drink plenty of water. Dehydration makes dizziness and fatigue worse.
- Go slow. If you’re sensitive, extend your taper to 6-8 weeks. Some people need months. There’s no rush. The goal is stability, not speed.
- Use liquid formulations. If your drug comes in liquid form (like sertraline or escitalopram), you can make tiny dose reductions-down to 1 mg or less. This gives you fine control.
- Ask about temporary help. If anxiety spikes during the switch, your doctor might suggest a short course of hydroxyzine or a low-dose benzodiazepine. This isn’t a long-term fix, but it can help you get through the toughest days.
When You Need to See Your Doctor
You don’t need to wait until your next scheduled appointment. If you experience any of these, call your provider right away:
- High fever, rapid heartbeat, stiff muscles, confusion, or seizures-these could be signs of serotonin syndrome.
- Thoughts of self-harm or suicide. This risk increases in the first few weeks after switching, especially for people under 25.
- Withdrawal symptoms that don’t improve after a few days or get worse.
- Severe dizziness or fainting.
Follow-up visits are part of the plan. Most guidelines say you should check in within 2 weeks of starting the new drug. For younger adults or those with a history of suicide risk, the first check-in should be at 1 week.
What’s New in Switching Antidepressants
Science is catching up to the real-world challenges of switching. One big advance is pharmacogenetic testing-like GeneSight. It looks at your genes to predict how your body will process certain antidepressants. In a 2022 trial, people who used this test had 28% higher remission rates. But it costs around $399 out-of-pocket in the U.S., so it’s not yet standard.
Another promising area is ultra-low-dose naltrexone. Early trials show it can reduce withdrawal symptoms by a third during SSRI switches. It’s still experimental, but it points to a future where switching isn’t just about patience-it’s about targeted support.
The Most Important Rule: You’re Part of the Decision
Switching antidepressants isn’t something your doctor does to you. It’s something you do together. The 2023 American Psychiatric Association guidelines say shared decision-making isn’t optional-it’s required. That means you need to know the risks, the options, and what to expect.
Ask questions:
- Why are we switching?
- What’s the plan? How long will it take?
- What side effects should I watch for?
- What do I do if I feel worse?
And if you’re unsure-say so. There’s no shame in asking for more time, a slower taper, or even trying therapy alongside medication. You’re not broken for needing to switch. You’re just human.
Real Talk: What Patients Say
On Reddit’s r/antidepressants, with over 250,000 members, people share their real experiences. The most common advice? Go slower than you think you need to. One person switched off paroxetine over 6 months using liquid drops. Another used a combination of melatonin and magnesium to sleep during the transition. A third said the hardest part wasn’t the physical symptoms-it was the fear that they’d never feel normal again.
But here’s the hopeful part: almost everyone who stuck with a careful plan eventually found something that worked. Not always on the first try. But they found it.
Final Thought: This Is a Process, Not a Mistake
Switching antidepressants doesn’t mean you’ve failed. It means you’re listening to your body. It means you’re not giving up-you’re adjusting. Depression is complex. Medications are tools, not magic. Sometimes you need a different tool. And that’s okay.
The goal isn’t to get off medication. The goal is to feel better. And that’s possible-even through the messy middle.

Chinmoy Kumar
February 1, 2026 AT 12:20Ansley Mayson
February 3, 2026 AT 01:18Bridget Molokomme
February 4, 2026 AT 21:32Gary Mitts
February 5, 2026 AT 22:58Hannah Gliane
February 7, 2026 AT 00:50Sandeep Kumar
February 8, 2026 AT 00:56Bob Hynes
February 8, 2026 AT 21:41Akhona Myeki
February 10, 2026 AT 18:08Marc Durocher
February 12, 2026 AT 13:16Eli Kiseop
February 12, 2026 AT 16:07Nick Flake
February 14, 2026 AT 08:33phara don
February 16, 2026 AT 04:16larry keenan
February 17, 2026 AT 10:07Becky M.
February 18, 2026 AT 08:26Brett MacDonald
February 18, 2026 AT 10:46