Sulfa Drug Allergies: What You Really Need to Know About Cross-Reactivity
People say they have a "sulfa allergy" all the time. But what does that actually mean? If you’ve been told you’re allergic to sulfa drugs, you might be avoiding medications you don’t need to. And worse-you could be taking riskier alternatives that aren’t better, just more expensive or more likely to cause side effects. The truth? Most people who think they’re allergic to sulfa aren’t allergic at all-or at least, not to the drugs they’re being told to avoid.
What Is a "Sulfa Allergy" Really?
When someone says they have a "sulfa allergy," they usually mean they had a bad reaction to an antibiotic like sulfamethoxazole (found in Bactrim or Septra). But "sulfa" isn’t a single thing. It’s a chemical group found in dozens of medications. The problem? Many of those drugs have nothing in common with the ones that cause real allergic reactions. The real issue is structural. Antibiotic sulfonamides-like sulfamethoxazole, sulfadiazine, and dapsone-have a specific part in their molecule called an arylamine group. When your body breaks these down, it creates a reactive compound that can trigger an immune response. That’s what causes true allergic reactions: rashes, hives, fever, or worse-Stevens-Johnson Syndrome. But here’s the key: non-antibiotic sulfonamides don’t have that same structure. Medications like hydrochlorothiazide (for high blood pressure), furosemide (a water pill), celecoxib (Celebrex for arthritis), and acetazolamide (for glaucoma) are chemically different. They don’t produce the same reactive metabolites. So even though they contain "sulfonamide" in their name, they’re not the same thing.How Common Are Real Sulfa Allergies?
About 3% of people in the U.S. say they have a sulfa allergy. But when doctors test them, only 1.5% to 2% actually have a true IgE-mediated reaction. The rest? They had a rash after taking an antibiotic, maybe felt nauseous, or were told they were allergic by a parent or a nurse decades ago. Some reactions were just side effects-not allergies at all. A 2003 study of over 17,500 people with documented sulfonamide antibiotic allergies found that their risk of reacting to non-antibiotic sulfonamides was basically the same as someone with no allergy at all. That’s right-9.5% of people without any sulfa allergy had a reaction to other drugs. So did 9.9% of people with a confirmed sulfa allergy. No difference. Meanwhile, the same study showed that people with a sulfa antibiotic allergy were 2.5 times more likely to react to another antibiotic in the same class. That’s the real cross-reactivity: between antibiotics, not between antibiotics and blood pressure pills.Which Medications Are Safe? Which Aren’t?
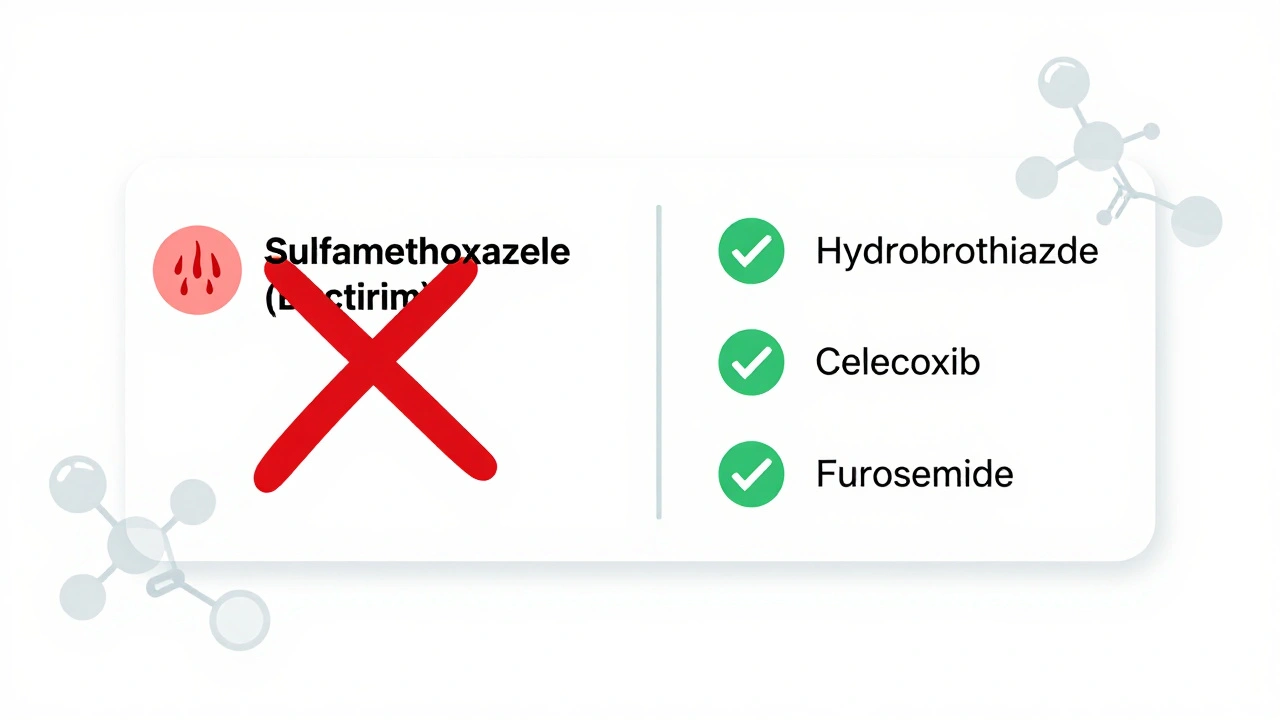
Let’s make this simple. Here’s what you need to know:- Avoid if you have a true sulfonamide antibiotic allergy: Sulfamethoxazole-trimethoprim (Bactrim, Septra), sulfadiazine, sulfacetamide (eye drops), dapsone.
- Generally safe: Hydrochlorothiazide (HCTZ), furosemide (Lasix), chlorthalidone, celecoxib (Celebrex), acetazolamide (Diamox), sulfonylureas like glyburide (for diabetes), torsemide.
- Use caution: Sulfasalazine (Azulfidine). This one’s tricky. It breaks down into sulfapyridine, which is an antibiotic sulfonamide. About 10% of people with sulfa antibiotic allergies react to it.
Why Does This Misunderstanding Exist?
For decades, doctors just wrote "sulfa allergy" in charts. No details. No context. Patients were told to avoid "all sulfa drugs." Pharmacists saw "sulfa allergy" and flagged everything with "sulf" in the name. Electronic health records didn’t distinguish between classes. So if you had a rash from Bactrim, you were blocked from taking your blood pressure pill, your glaucoma drops, even your arthritis medicine. The result? People go years without needed medications. One patient in Seattle avoided hydrochlorothiazide for 15 years because of a childhood rash. Her blood pressure was poorly controlled. Another was denied furosemide for heart failure because her old chart said "sulfa allergy." Her swelling got worse. A 2021 study found that pharmacist-led reviews cut unnecessary sulfa restrictions by nearly 70% across 12 hospitals. That’s because pharmacists asked: "Which drug caused the reaction? Was it an antibiotic?" And then they checked the actual chemical structure.What Should You Do If You Think You’re Allergic?
If you’ve been told you have a sulfa allergy, here’s what to do:- Find out what actually happened. Was it a rash? Fever? Blistering? Did you need hospitalization? Mild rashes are often not allergic. Severe reactions like SJS or TEN mean you should avoid all antimicrobial sulfonamides.
- Ask for clarification. Tell your doctor: "I was told I’m allergic to sulfa. But which drug caused it?" If it was Bactrim or Septra, you likely don’t need to avoid HCTZ or Celebrex.
- Consider a drug challenge. For mild reactions, your doctor can give you a single dose of hydrochlorothiazide or celecoxib under observation. In one study, 98.7% of patients with "sulfa allergy" tolerated it without issue.
- Update your records. Don’t let your chart say "sulfa allergy." It should say "allergy to sulfamethoxazole-trimethoprim" or "no known sulfa antibiotic allergy." Precision saves lives.

The Bigger Picture: Cost, Safety, and Stewardship
This isn’t just about convenience. It’s about safety and cost. When people are wrongly labeled as allergic to sulfa drugs, doctors often turn to broader-spectrum antibiotics like fluoroquinolones (Cipro, Levaquin) to treat UTIs. But those drugs carry a higher risk of C. difficile infection-nearly twice as likely. They’re also more expensive and can cause tendon damage or nerve problems. The Agency for Healthcare Research and Quality estimates that incorrect sulfa allergy labels cost the U.S. healthcare system over $1.2 billion a year. That’s from longer hospital stays, more expensive drugs, and unnecessary testing. The CDC says better allergy documentation could save $850 million annually just by allowing safer, more targeted antibiotic use. Hospitals like those using Epic’s 2022 system have cut wrong allergy flags by 42% just by splitting "sulfa allergy" into two categories: antibiotic and non-antibiotic.What’s Changing Now?
The medical world is waking up. The FDA now requires drug labels to clearly distinguish between antimicrobial and non-antimicrobial sulfonamides. The American Academy of Allergy, Asthma & Immunology says there’s no significant cross-reactivity. The Cleveland Clinic, Mayo Clinic, and American College of Rheumatology all say it’s safe to use celecoxib and HCTZ in patients with sulfonamide antibiotic allergies. New research is even helping us identify true allergies with blood tests. By detecting IgE antibodies to the hydroxylamine metabolite, labs can now confirm sulfa antibiotic allergy with over 94% accuracy. This isn’t science fiction-it’s happening in clinics right now.Bottom Line: Don’t Assume. Ask. Verify.
If you’ve been told you’re allergic to sulfa, don’t take it at face value. You might be avoiding safe, effective, and cheaper medications because of a label that’s outdated or inaccurate. Talk to your doctor. Ask what drug caused the reaction. Check the chemical structure. Get tested if needed. The goal isn’t to ignore allergies. It’s to treat them correctly. A true allergy to sulfamethoxazole? That matters. A blanket "sulfa allergy" that keeps you from your blood pressure pill? That’s a mistake-and it’s preventable.Is it safe to take hydrochlorothiazide if I have a sulfa allergy?
Yes, it’s generally safe. Hydrochlorothiazide is a non-antibiotic sulfonamide and does not contain the arylamine group that triggers allergic reactions in sulfonamide antibiotics like Bactrim. Studies show no increased risk of reaction in people with confirmed sulfonamide antibiotic allergies. The FDA and major medical societies confirm this distinction.
Can I take Celebrex if I’m allergic to sulfa?
Yes. Celecoxib (Celebrex) is a non-antibiotic sulfonamide. Multiple studies, including one from the Mayo Clinic, show no increased risk of allergic reaction in patients with sulfonamide antibiotic allergies. The American College of Rheumatology specifically recommends it as a safe option for arthritis patients with sulfa allergies.
Does a sulfa allergy mean I can’t take any medication with "sulf" in the name?
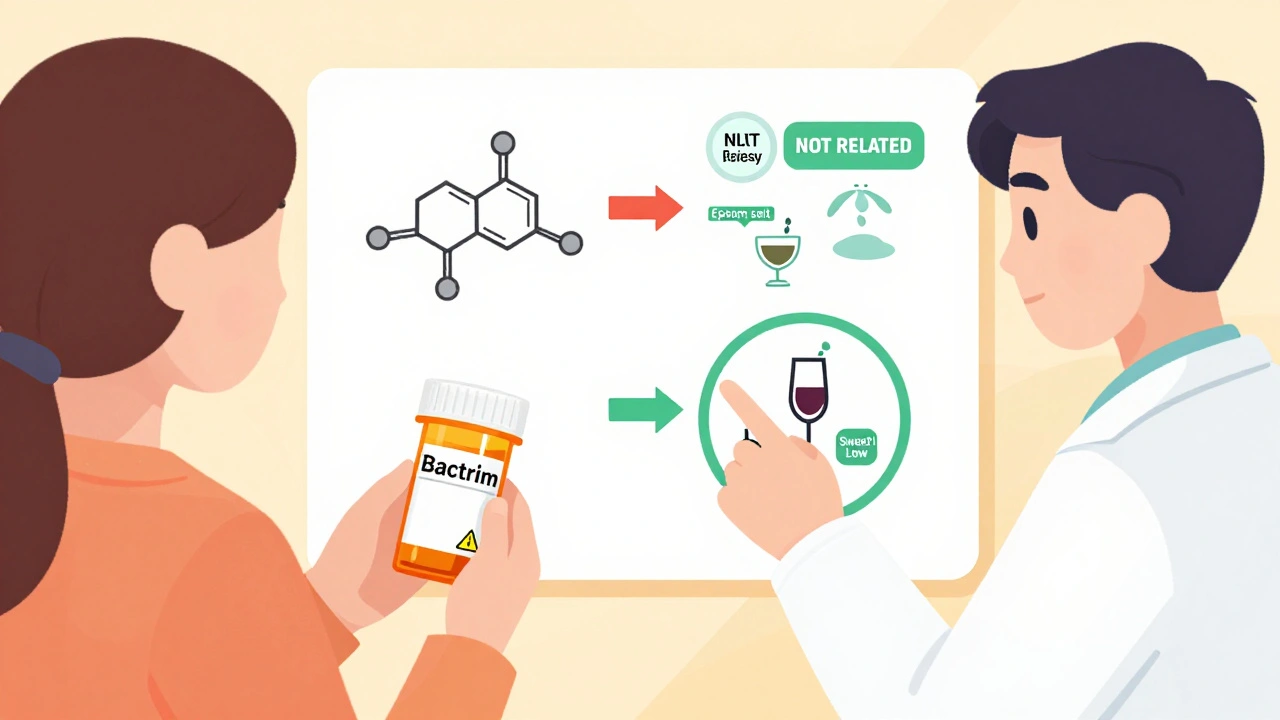
No. Sulfates (like magnesium sulfate in Epsom salt), sulfites (in wine), and sulfonamides are chemically different. A sulfa allergy only applies to specific antibiotic drugs with an arylamine group. Avoiding all "sulf"-containing substances is unnecessary and can limit your treatment options.
What should I do if I had a rash after taking Bactrim?
If it was a mild rash without fever, blistering, or breathing trouble, you may not have a true allergy. Talk to your doctor about a supervised challenge with a non-antibiotic sulfonamide like hydrochlorothiazide. Over 98% of people with mild reactions pass this test. If it was severe (like blistering skin or trouble breathing), avoid all antimicrobial sulfonamides but still ask about non-antibiotic options.
How can I get my allergy label corrected in my medical records?
Ask your primary care doctor or allergist to review your history. Request a specific update: change "sulfa allergy" to "allergy to sulfamethoxazole-trimethoprim" or "no known sulfa antibiotic allergy." Bring evidence from your past reactions. Pharmacists can also help-many hospital systems now have pharmacist-led allergy clarification programs.
Is there a blood test for sulfa allergy?
Yes. Component-resolved diagnostics can detect IgE antibodies to the hydroxylamine metabolite produced by antimicrobial sulfonamides. These tests are over 94% accurate in confirming true sulfa antibiotic allergies and are becoming available in specialty allergy clinics. They help distinguish real allergies from false labels.
Why do some doctors still say all sulfa drugs are unsafe?
Many doctors were trained decades ago when the distinction wasn’t well understood. Electronic health records still use vague labels. A 2023 survey found 67% of primary care physicians incorrectly believe non-antibiotic sulfonamides should be avoided. Education is improving, but misinformation persists. Don’t rely on outdated assumptions-ask for the latest evidence.

Geraldine Trainer-Cooper
December 7, 2025 AT 10:31So basically if you got a rash from Bactrim in 2003 you’re now banned from all meds with sulf in the name? That’s wild. My grandma’s chart still says "sulfa allergy" and she’s on HCTZ and celecoxib and has been for 12 years. No issues. People just copy-paste labels like it’s gospel.
Myles White
December 7, 2025 AT 17:00I work in pharmacy and this is the most common mislabeling I see. Patients come in with "sulfa allergy" flagged and we have to go through their entire history-was it a rash? Did they have a fever? Was it Bactrim? Most times it’s just a side effect or a viral rash coinciding with antibiotics. We’ve started asking patients to describe the reaction instead of just accepting "allergy" as fact. It’s saved so many people from being denied effective meds. Still, EHRs are garbage at distinguishing between antibiotic and non-antibiotic sulfonamides. It’s all just one checkbox. Someone needs to fix that.
Jackie Petersen
December 8, 2025 AT 16:10Of course the FDA and Mayo Clinic say it’s fine. But who controls the labs? Who controls the data? This is all part of the pharmaceutical industry’s plan to push expensive brand-name drugs. HCTZ costs pennies. Celebrex? Hundreds. They want you scared of the cheap stuff so you’ll take the profitable ones. Don’t be fooled. There’s a reason they don’t want you asking questions.
Karen Mitchell
December 9, 2025 AT 06:05This article is dangerously misleading. You’re telling people to ignore decades of medical warnings based on some vague chemical distinction? What if the immune system reacts differently in each individual? You’re playing with people’s health. And you call this science? This is reckless. I’ve seen patients develop anaphylaxis after being told "it’s safe." You’re not a doctor. You’re a marketing pamphlet.
Nava Jothy
December 10, 2025 AT 14:53OMG I’ve been avoiding ALL sulf- meds since I got a rash on Bactrim in college 😭 Now I’m told I can take my glaucoma drops?? My eyes have been burning for 8 years bc I was too scared to ask… I’m crying rn. Thank you for this. 🙏❤️
brenda olvera
December 11, 2025 AT 06:03As someone who grew up in a household where "sulfa" meant "never again"-I’m so glad this info is out there. My mom refused to let me take any diuretic for years because of a childhood reaction. Now I’m on HCTZ and my blood pressure is normal for the first time since I was 20. Education saves lives. Thank you for writing this.
olive ashley
December 12, 2025 AT 07:16Let me guess-this was funded by Big Pharma. Who benefits from people thinking they can take Celebrex? The same companies that make the expensive alternatives. The real danger isn’t the label-it’s the corporate push to reclassify allergies so they can sell more pills. And now you’re giving people permission to gamble with their immune systems. Congrats.
Chris Park
December 13, 2025 AT 23:05There’s a reason doctors avoid non-antibiotic sulfonamides in patients with sulfa allergies: because the data is inconclusive. You cite a 2003 study like it’s definitive, but multiple meta-analyses show variable cross-reactivity depending on patient genetics, metabolic pathways, and co-morbidities. To say it’s "safe" is an overstatement. Medicine isn’t binary. You’re oversimplifying a complex immunological phenomenon for clicks.
Brooke Evers
December 14, 2025 AT 22:15I’ve had patients cry in my office because they were told they couldn’t take their arthritis meds or blood pressure pills for 20 years. One woman was on three different antibiotics for her UTI because she was "allergic to sulfa"-and they all gave her stomach cramps. We did a supervised challenge with HCTZ. No reaction. She’s been stable since. This isn’t just about chemistry-it’s about dignity. People deserve to be treated like individuals, not labels.
joanne humphreys
December 16, 2025 AT 04:20I love how this breaks down the difference between sulfonamides, sulfates, and sulfites. I used to avoid wine and Epsom salts because I thought I was allergic to "sulfa." I had no idea they were chemically unrelated. This is the kind of info that should be taught in high school biology. Thank you for making it so clear.
Akash Takyar
December 16, 2025 AT 16:28As a physician in India, I see this daily. Patients come in with handwritten notes from decades ago: "Allergic to sulfa-avoid all drugs." We have to dig through old charts, talk to relatives, sometimes even call previous clinics. The lack of specificity is dangerous. We now have a protocol: if the reaction was mild and not to a sulfonamide antibiotic, we proceed with caution and document the exact drug. Precision is not a luxury-it’s a necessity.
Andrew Frazier
December 18, 2025 AT 06:39Yeah right. Next they’ll say penicillin allergies are fake too. You think the FDA gives a damn about your little chemical distinctions? They’re in bed with the drug companies. And you’re just some guy with a blog trying to sell people on expensive generics. Wake up. The system doesn’t want you healthy-it wants you dependent.
Ibrahim Yakubu
December 19, 2025 AT 08:50Wait. So if I had a rash from Bactrim, I can now take my arthritis pill? My cousin in Lagos just died because they gave him Celebrex after he had a reaction to sulfamethoxazole. You think that’s a coincidence? You think science is that simple? You’re playing with lives. This isn’t a blog post-it’s a death sentence waiting to happen.
Saketh Sai Rachapudi
December 21, 2025 AT 05:16Ugh this is why America is falling apart. You let people ignore medical warnings because of some fancy study? My uncle had a bad reaction to sulfa and now he’s fine because he avoided everything. You think your fancy science matters when real people get hurt? Stop pushing your liberal agenda. Trust the old ways.