Steroids and NSAIDs Together: Why This Combo Raises GI Bleeding Risk and How to Prevent It
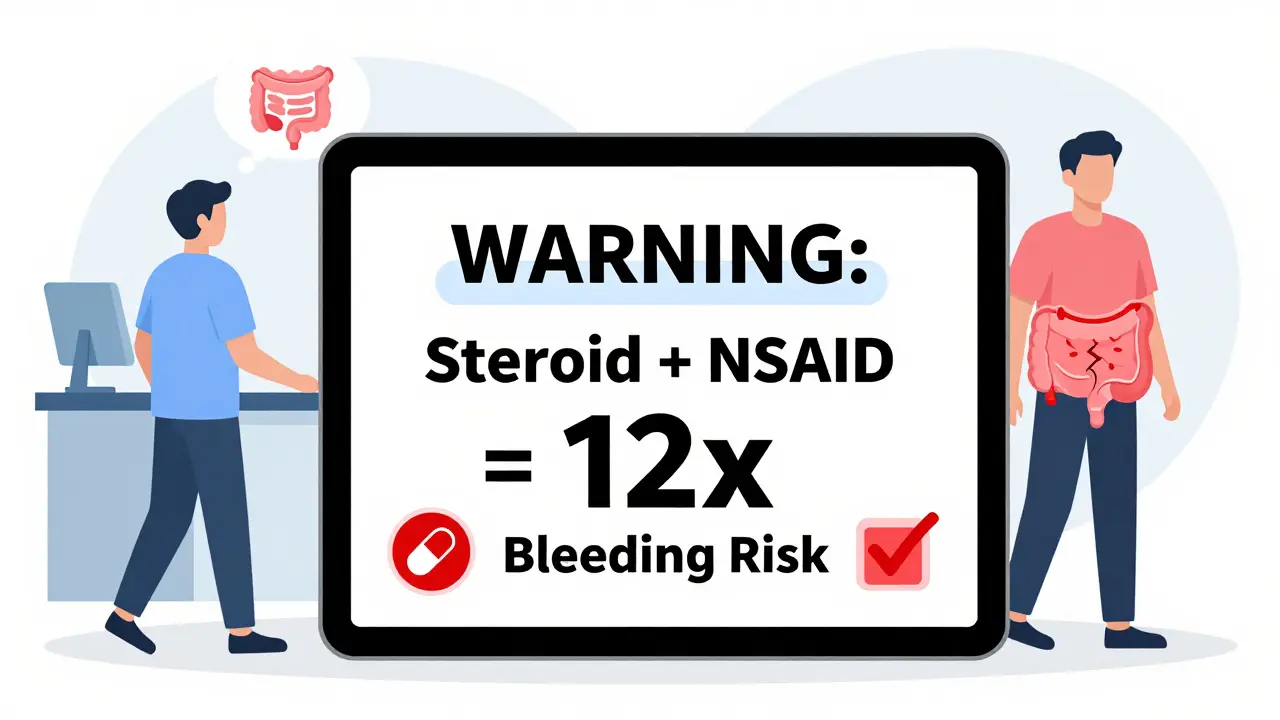
When you’re on steroids like prednisone and also taking ibuprofen or naproxen for pain or inflammation, you might think you’re just managing two common conditions. But what you don’t realize is that you’re putting yourself at serious risk - one that many doctors still overlook. The combination of systemic corticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs) doesn’t just add risks. It multiplies them. And the result? A gastrointestinal (GI) bleeding risk that can be more than 12 times higher than if you took either drug alone.
Why This Combo Is So Dangerous
NSAIDs hurt your stomach in two ways. First, they irritate the lining directly. Second, and more importantly, they block an enzyme called COX-1. That enzyme helps make prostaglandins - chemicals that protect your stomach lining by boosting mucus, blood flow, and healing. Without them, your stomach is vulnerable. Even a small ulcer can turn into a life-threatening bleed. Steroids make this worse. They don’t just add to the damage. They hide it. Steroids reduce inflammation, so if you develop an ulcer, you might not feel the usual warning signs like burning pain or nausea. By the time you notice bleeding - maybe through black, tarry stools or vomiting blood - it’s already serious. Steroids also slow down healing. An ulcer that might have closed on its own in a week can linger for weeks, growing deeper and more likely to rupture. Studies show the numbers don’t lie. If you take an NSAID alone, your risk of upper GI bleeding goes up about fourfold. Add steroids, and that risk jumps to an odds ratio of 8.9. For people on high-dose NSAIDs (like ibuprofen over 1,200 mg a day), the risk skyrockets to over 12 times higher. And if you’re also on blood thinners like warfarin? That number climbs even further - past 13 times the baseline risk.It’s Not Just Peptic Ulcers
Most people think GI bleeding means a stomach ulcer. But nearly one-third of NSAID-related bleeds happen in the lower GI tract - the colon or small intestine. These are harder to detect, often showing up as sudden anemia or unexplained fatigue. And if you’re on steroids, your body’s natural warning signals are muted. You might feel fine until you collapse from internal blood loss. A 1999 study found that 86% of patients with lower GI bleeds had taken NSAIDs. That’s not a coincidence. It’s a pattern. And when steroids are in the mix, the damage spreads. The mucosal lining weakens everywhere - not just in the stomach, but along the entire digestive tract.Not All NSAIDs Are Created Equal
Some NSAIDs are worse than others. Traditional ones like naproxen, diclofenac, and high-dose ibuprofen carry the highest risk. They hit both COX-1 and COX-2 enzymes, wiping out the protective prostaglandins. COX-2 selective drugs like celecoxib were designed to avoid this. They spare COX-1, so they’re gentler on the stomach. Trials like CLASS and VIGOR showed COX-2 inhibitors cut upper GI bleeding risk by 50-60% compared to traditional NSAIDs. But here’s the catch: even celecoxib isn’t safe when combined with steroids. The risk is lower than with naproxen, but it’s still there. And if you’re over 65, have a history of ulcers, or are on blood thinners? That’s not a minor concern. That’s a red flag.
What You Need to Do: PPIs Are Non-Negotiable
The only proven way to protect yourself is with a proton pump inhibitor (PPI). That’s a drug like omeprazole, esomeprazole, or pantoprazole. These drugs shut down stomach acid production, giving your lining a chance to heal. Guidelines from the American College of Gastroenterology and the American Gastroenterological Association are clear: if you’re taking both an NSAID and a steroid, you must also take a PPI. Not an H2 blocker like famotidine. Not just “taking it with food.” A PPI. Period. Why? Because PPIs reduce NSAID-induced ulcers by 73%. H2 blockers? Only 48%. That’s a huge difference. And the effect is even stronger when you’re on high-dose NSAIDs or have prior ulcer history. In those cases, doctors should prescribe double the standard dose - like 40 mg of omeprazole instead of 20 mg. The evidence is so strong that the European Society of Gastrointestinal Endoscopy says: if you’ve had a past ulcer, you should never get NSAIDs and steroids together unless you’re on a PPI. And even then, you need close monitoring.Why So Many People Still Get Hurt
You’d think this would be standard practice. But it’s not. A 2022 study of over 12,000 hospital patients found that only 39% of those on both steroids and NSAIDs got a PPI. In non-rheumatology departments - like primary care or emergency rooms - that number dropped to 22%. Why? Because many doctors don’t know the risk. Or they assume the patient is fine because they’re only on a “short steroid burst.” That’s a dangerous myth. Research shows the risk spikes within just seven days of starting the combo. A 5-day prednisone course for a sinus infection? If you’re also taking ibuprofen for a sore knee? You’re already in danger. The FDA has boxed warnings on NSAIDs for GI bleeding. But they don’t mention steroids. So most patients never hear about the combo risk. A 2023 survey by the NSAID Injury Foundation found that 63% of patients who suffered a bleed had no warning from their doctor.What to Ask Your Doctor
If you’re prescribed steroids and you’re already taking an NSAID - even an over-the-counter one - ask these questions:- Am I at risk for GI bleeding from this combo?
- Should I be on a PPI? Which one, and for how long?
- Can we switch to a safer NSAID like celecoxib?
- Is there an alternative to NSAIDs - like acetaminophen or physical therapy - that won’t hurt my gut?
New Tools Are Helping - But Only If Used
There’s good news. In 2023, the FDA approved Vimovo - a single pill that combines naproxen with esomeprazole. It’s designed for high-risk patients. Studies show it cuts endoscopic ulcers by 54% compared to naproxen alone. Some health systems are making changes too. Kaiser Permanente and Mayo Clinic now have automatic alerts in their electronic records: if a doctor prescribes prednisone and ibuprofen together, the system pops up a warning and suggests a PPI. At Mayo, this cut GI bleeds by nearly 70%. But outside integrated systems? Most clinics still rely on memory. And memory fails.What You Can Do Right Now
If you’re on steroids and NSAIDs:- Stop taking NSAIDs if you can. Use acetaminophen for pain instead - it doesn’t affect the stomach lining.
- If you must keep the NSAID, ask for a PPI. Don’t wait for symptoms.
- Don’t take OTC NSAIDs without telling your doctor. Many people don’t realize daily ibuprofen counts.
- Watch for signs of bleeding: black stools, vomiting blood, dizziness, or sudden fatigue.
- If you’ve had a past ulcer, don’t take this combo without PPI - even for a few days.
The Bottom Line
This isn’t a rare side effect. It’s a predictable, preventable disaster. Every year, over 21 million Americans get NSAID prescriptions. Nearly a third of them also get steroids. That’s millions of people walking around with a ticking time bomb in their gut. The fix is simple: PPIs. The failure is human: forgetfulness, lack of awareness, and outdated assumptions. But you don’t have to be part of the statistic. Ask the right questions. Demand protection. Your stomach isn’t just a side effect - it’s your life.Can I take ibuprofen with prednisone if I take it with food?
No. Taking NSAIDs with food doesn’t protect your stomach from the damage caused by combining them with steroids. Food may reduce mild irritation, but it doesn’t stop the systemic suppression of protective prostaglandins. The only reliable protection is a proton pump inhibitor (PPI), like omeprazole. Even then, the risk remains elevated - so avoid the combo if possible.
Are COX-2 inhibitors like celecoxib safe with steroids?
They’re safer than traditional NSAIDs like naproxen, but not risk-free. Studies show celecoxib cuts upper GI bleeding risk by about half compared to older NSAIDs. But when combined with steroids, the risk still increases significantly - especially in older adults or those with prior ulcers. Always pair celecoxib with a PPI if you’re on steroids. Never assume it’s safe on its own.
How long should I take a PPI with steroids and NSAIDs?
You should take the PPI for the entire time you’re on both medications - and for at least two weeks after you stop the NSAID. Steroids can delay healing even after you stop taking them. If you’re on long-term NSAIDs (like for arthritis), your doctor may recommend continuing the PPI indefinitely. Don’t stop the PPI just because you feel fine - ulcers can form without symptoms.
I only took prednisone for 5 days. Do I still need a PPI?
Yes - if you’re also taking an NSAID. Research shows the risk of GI bleeding rises within 7 days of starting the combination. A short steroid burst doesn’t make you safe. In fact, many preventable bleeds happen during these brief courses because patients and doctors assume it’s low-risk. Always use a PPI if you’re combining steroids with NSAIDs, no matter how short the course.
What are the signs of a GI bleed from this combo?
Watch for black, tarry stools (melena), vomiting blood or material that looks like coffee grounds, sudden dizziness, rapid heartbeat, or unexplained fatigue and weakness. These can be signs of internal bleeding. Lower GI bleeds might show up as bright red blood in stool or sudden anemia. If you notice any of these, stop the NSAID and seek medical help immediately - even if you feel fine otherwise.
Can I use acetaminophen instead of NSAIDs while on steroids?
Yes - and it’s often the best choice. Acetaminophen (Tylenol) doesn’t affect prostaglandins or the stomach lining, so it doesn’t increase GI bleeding risk. It’s not as strong as NSAIDs for inflammation, but it’s effective for pain and fever. For many people on steroids, switching to acetaminophen is the safest way to manage discomfort without adding danger.
Is this risk only for prescription NSAIDs, or do OTC ones count too?
OTC NSAIDs count just as much. Daily ibuprofen (Advil), naproxen (Aleve), or aspirin taken regularly can be just as dangerous as prescription versions when combined with steroids. Many patients don’t realize that taking 200 mg of ibuprofen twice a day for back pain is a chronic NSAID use - not occasional use. That’s enough to raise your risk significantly. Always tell your doctor about any OTC pain meds you’re taking.

Fabio Raphael
December 26, 2025 AT 18:19I’ve been on prednisone for my autoimmune condition and ibuprofen for my back pain for months. No one ever warned me about this combo. I just thought the stomach upset was normal. Now I’m terrified. I’m calling my doctor tomorrow to get a PPI prescription. This post literally saved me.
Peter sullen
December 28, 2025 AT 10:10It is imperative to underscore, with rigorous clinical precision, that the synergistic pharmacodynamic interaction between systemic corticosteroids and non-selective COX inhibitors results in a statistically significant, multiplicative elevation in the incidence of upper and lower gastrointestinal hemorrhage-particularly in populations exhibiting comorbidities such as advanced age, prior peptic ulcer disease, or concomitant anticoagulant therapy. The data, as presented, is unequivocal and mandates adherence to ACG/AGA guidelines.
Amy Lesleighter (Wales)
December 29, 2025 AT 00:45Becky Baker
December 29, 2025 AT 07:42Ugh, another overblown medical scare post. My grandpa took ibuprofen and steroids for years and lived to 92. You people act like every pill is a death sentence. Just stop being so paranoid.
Rajni Jain
December 30, 2025 AT 06:35Thank you for sharing this. I’m from India and here, doctors rarely talk about GI risks. I’m on prednisone for my asthma and take ibuprofen for headaches. I didn’t know OTC counts too. I’m switching to acetaminophen today. You’re right-we need to speak up. You’re not alone.
Natasha Sandra
January 1, 2026 AT 01:23OMG I just started prednisone and was about to pop 2 Advil for my headache 😱 THANK YOU for this!! I’m grabbing omeprazole right now 💪❤️ #StaySafe #PPIisLife
Erwin Asilom
January 1, 2026 AT 03:20Becky Baker’s comment reflects a dangerous misconception. While anecdotal longevity exists, population-level epidemiological data demonstrates a clear, dose-dependent risk increase. The absence of symptoms does not equate to absence of pathology. The 2022 study cited shows a 78% under-prescription rate of PPIs in non-specialist settings. This is a systemic failure, not an individual overreaction.
Sumler Luu
January 3, 2026 AT 01:41Erwin is right. I’m a nurse, and I’ve seen three patients bleed out from this exact combo. One was 42, on a 5-day steroid course for bronchitis and daily Aleve for tennis elbow. No one asked about OTC meds. The warning should be on every prescription label. We need better systems-not just better patients.