Statin Intolerance Clinics: Structured Protocols to Reduce Side Effects
Statin Intolerance Assessment Tool
This assessment is based on the National Lipid Association's definition of statin intolerance: inability to tolerate at least two different statins at the lowest dose or any dose due to side effects. Results are for informational purposes only and should not replace professional medical advice.
For millions of Americans taking statins to lower cholesterol, these drugs are life-saving. But for some, the side effects are too much to bear. Muscle pain, weakness, cramps - symptoms that start quietly and grow worse over weeks. Many patients are told to stop statins altogether, thinking there’s no other way. But what if there’s a better path? Statin intolerance clinics are changing that story - not by avoiding statins entirely, but by rethinking how they’re used.
What Really Counts as Statin Intolerance?
Statin intolerance isn’t just feeling sore after a workout. The National Lipid Association (NLA) defines it clearly: you can’t tolerate at least two different statins - one at the lowest dose, another at any dose - because of side effects. But here’s the twist: most people who think they’re intolerant aren’t. Studies show only 5% to 15% of patients reporting muscle pain actually have true statin-associated muscle symptoms (SAMS). The rest? Their symptoms often come from something else - low vitamin D, thyroid issues, or even the nocebo effect, where just expecting side effects makes you feel them.
That’s why structured clinics don’t jump to stop statins. They start by ruling out other causes. Before anything else, they check thyroid levels, vitamin D, and drug interactions. A patient on simvastatin might also be taking a supplement like CoQ10 or red yeast rice - both can worsen muscle symptoms. A simple blood test for creatine kinase (CK) can help too. If CK is over 7 times the upper limit of normal, or above 1,000 IU/L, that’s a red flag. But if CK is normal and symptoms are mild? That’s a clue the problem might not be the statin at all.
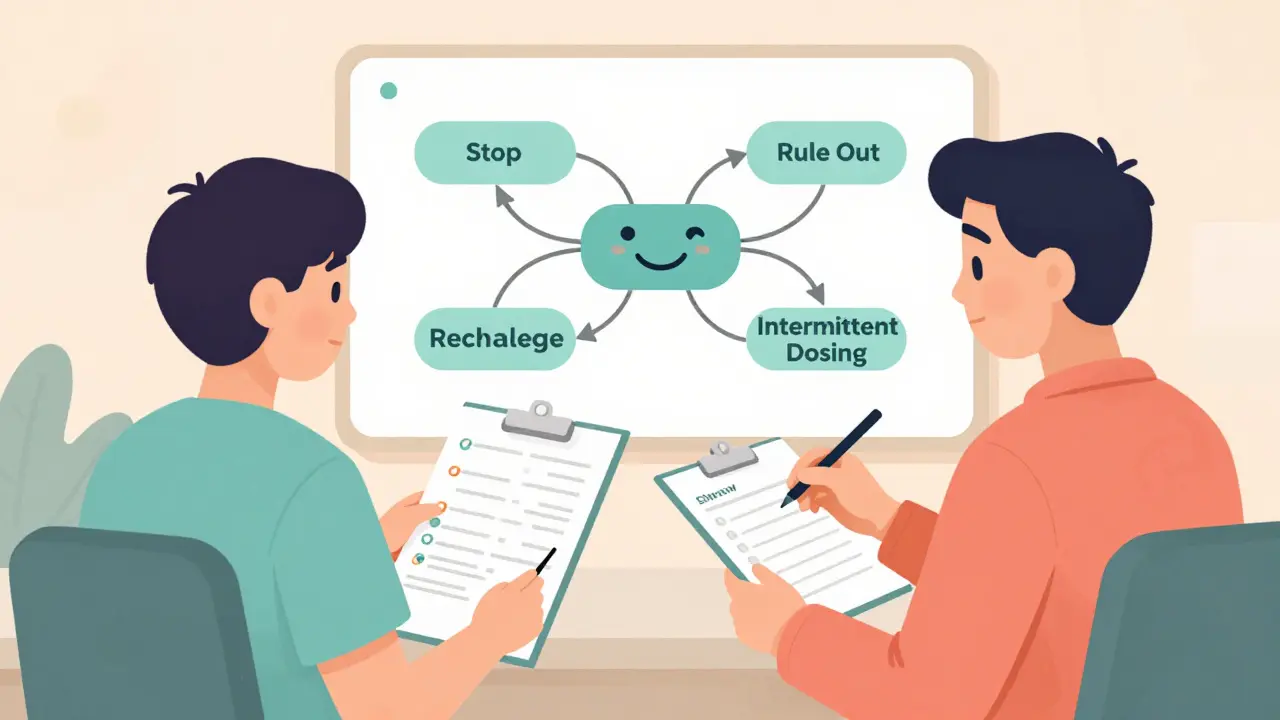
The Four-Step Protocol: How Clinics Reclaim Statin Therapy
Statin intolerance clinics follow a strict, step-by-step process. It’s not guesswork. It’s science. Here’s how it works:
- Stop the statin - For two weeks, the patient stops all statins completely. Symptoms are tracked daily using a 0-10 pain scale. Muscle pain should begin to fade during this break.
- Rule out other causes - Blood tests check for thyroid problems, low vitamin D, kidney function, and drug interactions. Alcohol use and certain supplements are also reviewed. If a patient has hypothyroidism or low vitamin D, fixing those first can eliminate symptoms without touching the statin.
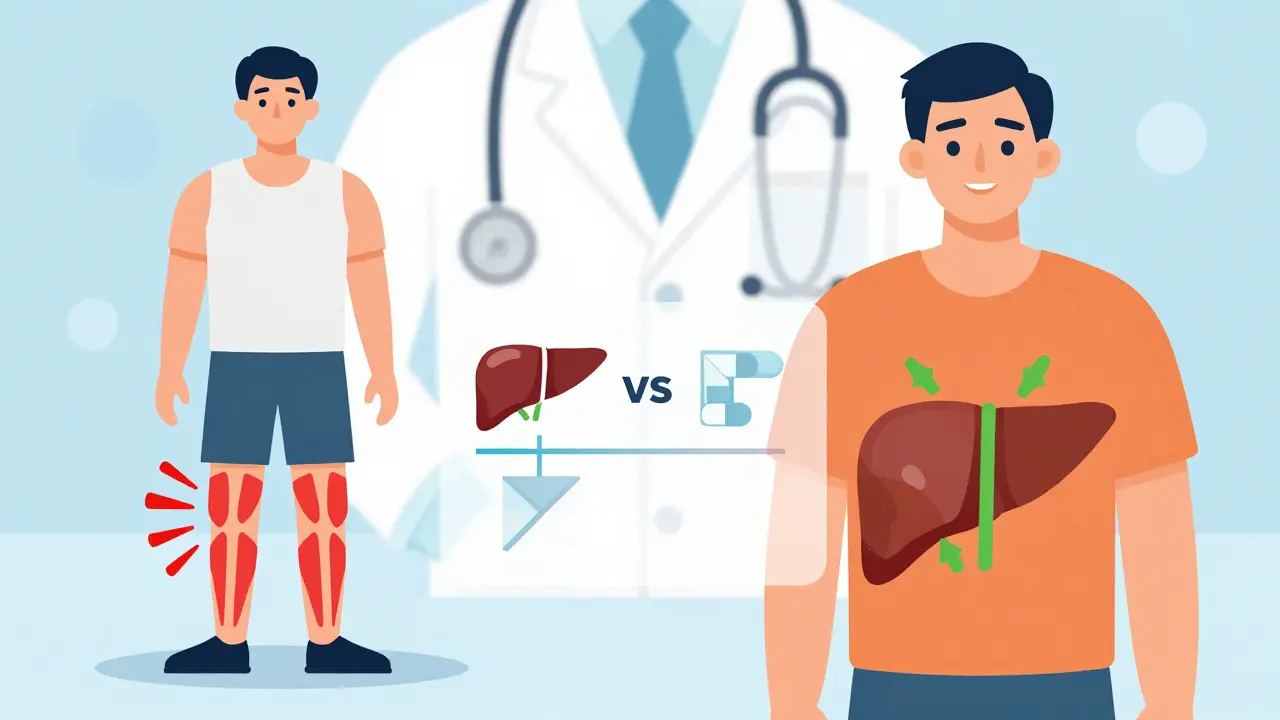
- Rechallenge with a different statin - This is where most clinics succeed. Instead of going back to the same statin, they switch to one with a different chemical profile. Lipophilic statins like simvastatin and atorvastatin spread into muscle tissue more easily. Hydrophilic statins like rosuvastatin and pravastatin are designed to target the liver. Switching to a hydrophilic statin works for 72% of patients who failed before.
- Try intermittent dosing - If daily dosing still causes issues, try every-other-day or twice-weekly dosing. Long-half-life statins like rosuvastatin or atorvastatin stay active in the body for days. A 2021 Cleveland Clinic study of 1,247 patients found 76% of those previously intolerant could tolerate rosuvastatin 5 mg twice a week. LDL cholesterol still dropped by 20-40%.
This approach cuts permanent statin discontinuation from 45% in general practice down to just 18% in clinics with structured protocols.
When Statins Just Won’t Work: Non-Statin Alternatives
Some patients truly can’t tolerate any statin - even at low or intermittent doses. That’s when non-statin therapies come in. The first-line choice? Ezetimibe. It blocks cholesterol absorption in the gut. It’s cheap - about $35 a month - and proven to cut major heart events by 6% in the IMPROVE-IT trial. It doesn’t cause muscle pain. Many patients who switch to ezetimibe after failing statins feel better immediately.
For higher-risk patients, bempedoic acid (Nexletol) is gaining traction. Approved by the FDA in 2020, it lowers LDL by about 18% without affecting muscle tissue. The CLEAR Outcomes trial with over 14,000 patients found no increase in muscle symptoms. It costs more - around $491 a month - but for those who can’t take statins, it’s a game-changer.
PCSK9 inhibitors like evolocumab and alirocumab are even more powerful, lowering LDL by 50-60%. But they’re expensive - over $5,850 a year - and insurance often denies them unless patients meet strict criteria. Some clinics help patients appeal these denials. One patient on Inspire’s forum spent 11 weeks and four appeals before getting approval. That’s not ideal, but it’s possible.
Why Most Doctors Still Miss This
Most primary care doctors don’t have the time or training to run a full statin rechallenge. They see a patient with muscle pain, stop the statin, and move on. No follow-up. No testing. No alternative plan. That’s why 18% of eligible patients still go untreated - not because statins don’t work, but because the system doesn’t know how to handle intolerance.
Specialized clinics fix this with teams. Pharmacists lead rechallenges. Dietitians help with lifestyle changes. Lipid specialists interpret lab results. At Cleveland Clinic, when pharmacists manage the process, outcomes improve by 22%. They know which statins to switch to, how to adjust doses, and when to add ezetimibe. They also use the ACC’s Statin Intolerance Tool, launched in March 2023, which calculates a patient’s 10-year heart attack risk and compares it to the risk of side effects. It turns guesswork into data-driven decisions.
Real Patient Stories - And What Works
One Reddit user, HeartPatient87, spent five years avoiding statins after severe muscle pain. At Johns Hopkins’ lipid clinic, they switched to rosuvastatin 5 mg twice a week with CoQ10. Within months, their LDL dropped from 142 to 89 - no pain.
Kaiser Permanente’s 2022 survey found 82% of patients in their program got back on lipid-lowering therapy. The top reasons? A clear plan and follow-up. Patients didn’t feel abandoned. They felt guided.
But not all stories are smooth. Wait times for these clinics average 6-8 weeks. Insurance hurdles for non-statin drugs are real. And some patients refuse to rechallenge - 31% of VA clinic patients won’t try another statin, even when told it might work. Fear is powerful.

The Future: Genetic Tests and New Delivery Systems
What’s next? Genetic testing. Mayo Clinic started screening for the SLCO1B1 gene variant in 2023. This variant increases the risk of simvastatin muscle damage by up to 400%. If you have it, you avoid simvastatin - and that’s it. No trial and error.
Even more exciting? Nanoparticle-delivered statins. In early trials (NCT04872662), these tiny statin packages target the liver directly, bypassing muscle tissue. Early results show 92% tolerability. If this works in larger trials, it could eliminate muscle side effects entirely.
Meanwhile, intermittent dosing is spreading fast. A 2024 ACC survey found 78% of lipid specialists plan to expand this approach. For patients who can’t take statins daily, it’s not a last resort - it’s the new standard.
How to Find a Statin Intolerance Clinic
If you’ve been told to stop statins and are scared of heart disease, ask your doctor: "Is there a lipid clinic nearby?" Most academic medical centers have them. Look for programs at hospitals affiliated with universities. The NLA’s online Statin Intolerance Management Toolkit (used by over 12,700 clinicians in 2024) lists participating centers. Medicare Part B now covers 80% of lipid specialist visits for this issue - so cost shouldn’t be a barrier.
Bring your symptom diary. List every statin you tried, when you started, what happened, and when it went away. Bring your latest blood work. Ask about ezetimibe or bempedoic acid. Don’t accept "just stop" as an answer. You have options. And they work.
Can you really tolerate statins after being labeled intolerant?
Yes - and many do. Studies show up to 80% of patients who think they’re intolerant can actually tolerate statins after a structured rechallenge. Most cases are misdiagnosed because symptoms weren’t properly tracked or other causes weren’t ruled out. A two-week break from statins, followed by switching to a hydrophilic statin like rosuvastatin or pravastatin, often resolves symptoms while keeping cholesterol under control.
Is ezetimibe a good alternative to statins?
Yes, and it’s often the first choice. Ezetimibe lowers LDL by about 15-20% and reduces major cardiovascular events by 6% based on the IMPROVE-IT trial. It doesn’t cause muscle pain, costs under $40 a month, and works well with low-dose statins. For patients who can’t tolerate statins, ezetimibe alone is a proven, safe, and affordable option.
Why do some statins cause more muscle pain than others?
It’s about how the drug moves through the body. Lipophilic statins like simvastatin and atorvastatin easily enter muscle tissue, which can trigger inflammation and pain. Hydrophilic statins like rosuvastatin and pravastatin are designed to be pulled into liver cells by transporters, staying mostly out of muscle. Switching from a lipophilic to a hydrophilic statin is the most effective way to reduce side effects - and it works for 72% of patients.
Does intermittent dosing really work?
Yes - and it’s backed by data. A 2021 study of 1,247 patients found 76% of those previously intolerant could tolerate rosuvastatin taken twice a week. LDL dropped 20-40%, and muscle pain disappeared. Long-half-life statins stay active for days, so you don’t need daily dosing. This approach is now recommended by the ACC and NLA as a first-line strategy for statin intolerance.
Are PCSK9 inhibitors worth the cost?
For high-risk patients who can’t take statins or ezetimibe, yes. PCSK9 inhibitors like evolocumab lower LDL by 50-60% and reduce heart attacks and strokes. But they cost over $5,800 a year. Insurance often denies them unless you’ve tried and failed at least two other therapies. Some clinics help patients appeal denials. If you have genetic heart disease, diabetes, or a history of heart attack, the long-term benefit may outweigh the cost.
What should I bring to my first statin intolerance clinic visit?
Bring a detailed symptom diary: when pain started, what statin you took, how severe it was (0-10 scale), and when it improved after stopping. Include all lab results - especially CK, thyroid, and vitamin D levels. List every medication and supplement you take. If you’ve tried multiple statins, write down which ones and what happened. The more detail you provide, the faster they can find a solution that works for you.
Statin intolerance isn’t a dead end. It’s a puzzle - and clinics now have the pieces to solve it. You don’t have to give up on statins. You just need the right system behind you.

Patrick Jarillon
February 7, 2026 AT 20:57AMIT JINDAL
February 9, 2026 AT 00:39Catherine Wybourne
February 10, 2026 AT 19:52Ariel Edmisten
February 11, 2026 AT 08:44Mary Carroll Allen
February 13, 2026 AT 00:28Eric Knobelspiesse
February 13, 2026 AT 21:57Ritu Singh
February 15, 2026 AT 17:02Mark Harris
February 17, 2026 AT 14:17Mayank Dobhal
February 18, 2026 AT 12:52Amit Jain
February 20, 2026 AT 02:27Savannah Edwards
February 21, 2026 AT 21:24Joey Gianvincenzi
February 23, 2026 AT 08:03Natasha Bhala
February 24, 2026 AT 09:33Gouris Patnaik
February 26, 2026 AT 00:33Jesse Lord
February 27, 2026 AT 14:34