SSRIs and NSAIDs Together: Why Your Risk of GI Bleeding Goes Up and How to Stay Safe
Every year, millions of people in the U.S. take SSRIs for depression or anxiety and NSAIDs for back pain, arthritis, or headaches. It seems harmless-two common meds, two common problems. But when you take them together, you’re not just adding risks. You’re multiplying them. And the result? A much higher chance of something dangerous: upper gastrointestinal bleeding.
How SSRIs and NSAIDs Work (and Why They’re Dangerous Together)
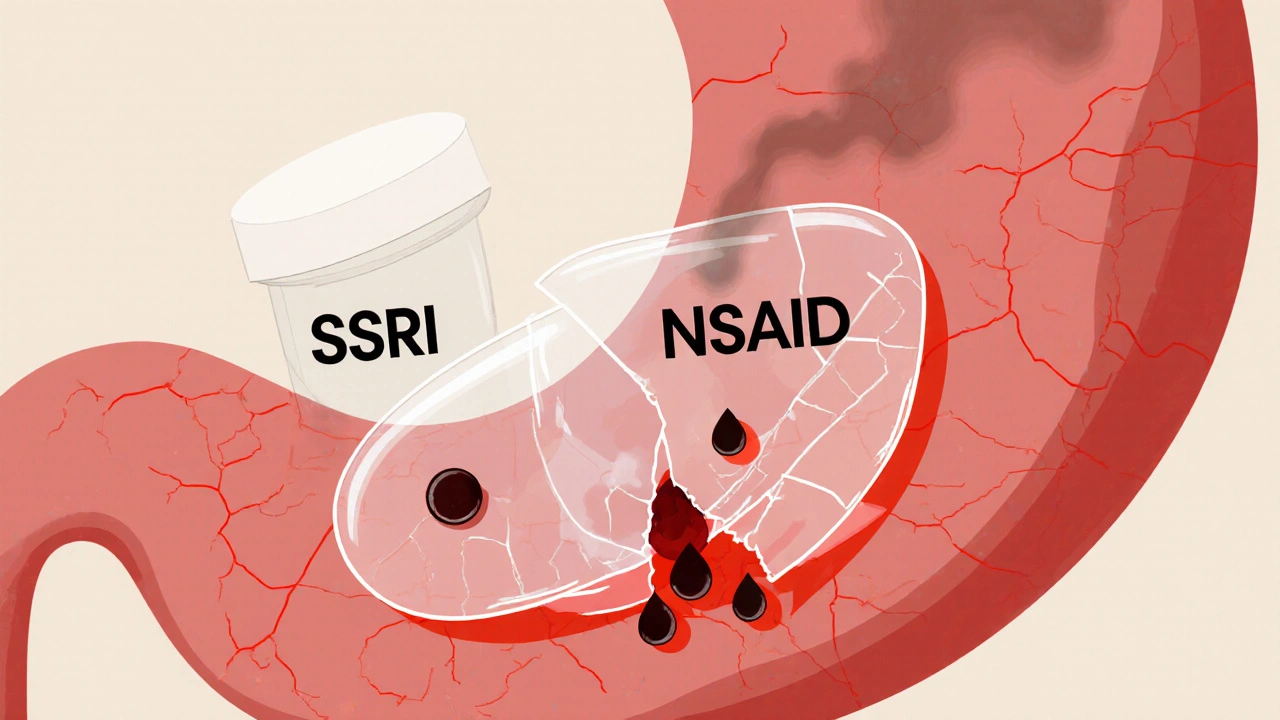
SSRIs like sertraline, fluoxetine, and citalopram help balance brain chemicals to lift mood. But they also affect platelets-tiny blood cells that stop bleeding. These drugs block serotonin from being taken back into platelets. That leaves platelets with less serotonin, which they need to clump together and seal small cuts in your stomach lining. Think of it like having fewer workers on a construction crew: when a tiny tear happens in your gut, your body can’t patch it fast enough.
NSAIDs like ibuprofen, naproxen, and diclofenac work by reducing inflammation and pain. But they do it by shutting down an enzyme called COX-1. That enzyme doesn’t just cause pain-it also makes prostaglandins, which protect your stomach lining. Without those, your stomach gets thinner, drier, and more vulnerable. Acid eats away at it. Small ulcers form. And if you’re already struggling to stop bleeding because of your SSRI? That’s when things turn serious.
The combination? It’s not 1+1=2. It’s more like 1+1=3.5. Studies show that taking both together raises your risk of upper GI bleeding by 75%. That’s not a small bump. That’s a major jump. And it’s not just theory. Real people are ending up in emergency rooms with black, tarry stools or vomiting blood because no one warned them this could happen.
Who’s Most at Risk?
Not everyone who takes SSRIs and NSAIDs will bleed. But some people are sitting on a ticking clock.
- People over 65: Your stomach lining naturally thins with age. Healing slows. Platelets don’t work as well. This group has the highest absolute risk.
- Those with a past ulcer or GI bleed: If you’ve had one before, you’re far more likely to have another-especially with these drugs.
- People on blood thinners: Warfarin, apixaban, or even daily low-dose aspirin? Add SSRIs and NSAIDs, and your bleeding risk skyrockets.
- Those with H. pylori infection: This common stomach bacteria causes ulcers. If it’s still active when you start these meds, your risk doubles.
A 2021 survey of over 1,200 primary care doctors found that less than 40% routinely checked for this interaction. That means most patients are left in the dark. If you’re on both meds and no one ever mentioned bleeding, you’re not alone. Sixty-eight percent of patients in a 2022 survey said they weren’t warned.
Which Medications Are Riskier?
Not all SSRIs or NSAIDs are created equal when it comes to bleeding risk.
For NSAIDs:
- High risk: Naproxen, diclofenac, piroxicam, ketorolac
- Lower risk: Ibuprofen (at standard doses)
- Safest option: Celecoxib (a COX-2 inhibitor)
Celecoxib doesn’t block COX-1 as much, so it’s gentler on your stomach. Studies show its bleeding risk is close to baseline-almost like not taking an NSAID at all. If you need an NSAID and you’re on an SSRI, celecoxib is the best choice.
For SSRIs:
Most SSRIs carry similar bleeding risks because they all affect platelet serotonin. But some data suggests escitalopram might be slightly safer than fluvoxamine or paroxetine. Still, don’t assume one SSRI is “safe.” The real issue isn’t which SSRI-it’s that you’re taking it with an NSAID.
What to Do Instead: Safer Alternatives
You don’t have to suffer pain or depression to stay safe. There are better paths.
For pain:
- Switch to acetaminophen (Tylenol). It doesn’t affect platelets or stomach lining. It’s not perfect for every kind of pain, but for headaches, muscle aches, or mild arthritis, it’s often enough.
- Try physical therapy, heat/cold therapy, or acupuncture. Many people reduce NSAID use by 50% or more with non-drug approaches.
- If you must use an NSAID, use the lowest dose for the shortest time possible.
For depression or anxiety:
- Consider bupropion (Wellbutrin). It doesn’t affect platelets. No bleeding risk. It’s not right for everyone, but for many, it’s a great alternative.
- Therapy, exercise, and sleep improvements can be powerful-sometimes enough to reduce or eliminate the need for medication.
One patient on Reddit shared that after switching from naproxen to celecoxib and adding omeprazole, they had zero GI issues for 18 months while staying on sertraline. That’s not luck. That’s smart management.
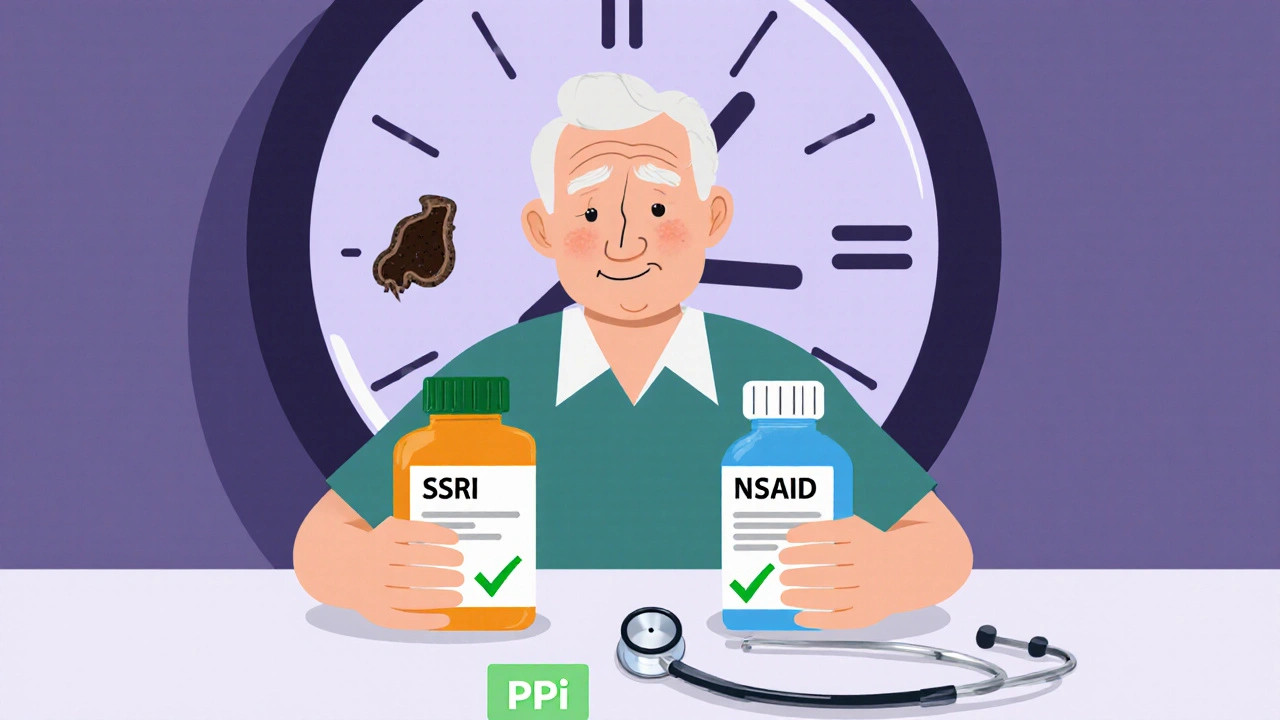
How to Protect Yourself: The Three-Step Plan
If you absolutely need both an SSRI and an NSAID, here’s what works:
- Take a proton pump inhibitor (PPI). Omeprazole (20mg daily), esomeprazole, or pantoprazole are the gold standard. Studies show PPIs cut the extra bleeding risk from this combo by 70%. That brings your risk back down near normal levels. Don’t skip this. It’s not optional if you’re on both meds.
- Get tested for H. pylori. If you have it, treat it. Eradicating this bacteria reduces ulcer risk by up to 80%. Most doctors don’t think to test unless you’ve had an ulcer-but if you’re on SSRIs and NSAIDs, you should be tested anyway.
- Monitor for warning signs. Black, tarry stools. Vomiting blood or material that looks like coffee grounds. Sudden dizziness or weakness. Abdominal pain that doesn’t go away. These aren’t normal. Go to the ER if you see them.
Some hospitals, like Cleveland Clinic, now have automated alerts in their electronic records that pop up when a doctor tries to prescribe both an SSRI and NSAID. Since 2020, they’ve seen a 42% drop in GI bleeding hospitalizations. That’s proof that systems work-but you can’t wait for your doctor’s system to catch up. Be your own advocate.
The Bigger Picture: Why This Keeps Happening
This isn’t a rare mistake. In 2022, a review of 2.1 million patient records found that nearly 3 out of 10 people on SSRIs were also prescribed NSAIDs within six months. That’s 9.8 million Americans at elevated risk. The FDA and EMA added warnings to drug labels years ago. But warnings don’t change behavior unless doctors are reminded-and patients are educated.
It’s also expensive. Upper GI bleeds from this interaction cost the U.S. healthcare system over $1.2 billion a year. Each hospitalization averages $15,642. That’s money spent on emergency care, blood transfusions, endoscopies, and ICU stays-all preventable.
Some companies are working on solutions. One new drug in Phase III trials combines ibuprofen with omeprazole in a single pill. That could make protection automatic. But until then, the solution is simple: know the risk, ask questions, and don’t accept “it’s fine” as an answer.
Final Takeaway: You Have Control
SSRIs and NSAIDs are powerful tools. But they’re not harmless. Taking them together without protection is like driving with a flat tire and no spare-you might make it to the store. But one bump, one stop, one stress, and you’re stranded in danger.
You don’t have to choose between managing your pain and your mood. You just need to manage them smarter. Ask your doctor: “Am I at risk for GI bleeding? Should I be on a PPI? Is there a safer pain reliever I can use? Could I switch to a different antidepressant?”
Most people assume their doctor already knows this. But the data shows they often don’t. Don’t wait for a hospital visit to learn the hard way. Have the conversation now. Your stomach will thank you.
Can I take ibuprofen with an SSRI if I’m on a PPI?
Yes, but only if you’re also taking a proton pump inhibitor (PPI) like omeprazole daily. Even though ibuprofen is one of the safer NSAIDs, combining it with an SSRI still increases bleeding risk. A PPI reduces that extra risk by about 70%. Never take ibuprofen and an SSRI together without a PPI unless your doctor has approved it after checking your personal risk factors.
Is celecoxib always safer than other NSAIDs when taking an SSRI?
Yes, based on current evidence. Celecoxib has a much lower risk of causing GI bleeding than non-selective NSAIDs like naproxen or diclofenac. Studies show its bleeding risk is close to baseline, especially when compared to drugs like ketorolac. However, celecoxib isn’t risk-free-it can still affect heart health in some people. Always discuss your full medical history with your doctor before switching.
Can I stop my SSRI if I need to take NSAIDs long-term?
Don’t stop your SSRI on your own. Stopping suddenly can cause withdrawal symptoms or a return of depression or anxiety. Instead, talk to your doctor about alternatives. Bupropion (Wellbutrin) is an antidepressant that doesn’t affect platelets and may be a safer option if you need ongoing NSAID use. Your mental health matters-just don’t trade one risk for another without a plan.
How long should I take a PPI if I’m on both meds?
If you’re taking both an SSRI and an NSAID long-term, you should generally take a PPI daily as long as you’re on both. For short-term NSAID use (like a week for a sprained ankle), a PPI may not be needed. But if you’re on NSAIDs for months or years-such as for arthritis-PPI therapy should be ongoing. Always review your need for both meds every 3-6 months with your doctor.
Are there natural ways to reduce GI bleeding risk while on these meds?
Yes, but they don’t replace medical protection. Avoid alcohol, quit smoking, and manage stress-these all worsen stomach lining damage. Eat regular meals, avoid spicy or acidic foods if they bother you, and don’t take NSAIDs on an empty stomach. But none of these replace a PPI if you’re on both an SSRI and NSAID. Natural methods help, but they don’t neutralize the drug interaction.
What if I already had a GI bleed while on these meds?
If you’ve had a GI bleed while on SSRIs and NSAIDs, you should avoid NSAIDs entirely unless absolutely necessary and only under strict medical supervision. Your doctor will likely recommend switching to acetaminophen for pain and possibly switching your antidepressant to one without platelet effects, like bupropion. You’ll also need long-term PPI therapy and regular follow-up. Future bleeding risk is very high-so this isn’t a situation to manage on your own.

Emily Barfield
November 2, 2025 AT 12:27So let me get this right: we’ve got a pharmaceutical-industrial complex that profits from stacking dangerous drug combinations, while patients are left to stumble through the minefield of side effects like it’s a game of Russian roulette with stomach acid??? And the solution? A proton pump inhibitor-another drug-because the system can’t be bothered to design safer alternatives or actually educate prescribers!!! This isn’t medicine-it’s corporate triage wrapped in a white coat.
Rebecca Parkos
November 3, 2025 AT 15:58I had no idea this was even a thing until my mom ended up in the ER last year. She was on sertraline for anxiety and ibuprofen for her knees. No one ever told her about the bleeding risk. She’s fine now, but I’m screaming at every doctor I see about this. If you’re on SSRIs and NSAIDs, ask for a PPI. Don’t wait for a black stool to wake you up.
Ted Carr
November 4, 2025 AT 17:01Wow. So the real takeaway is: doctors are lazy, patients are dumb, and the only thing keeping us alive is a $3 pill that no one tells us to take. Brilliant. Just brilliant. I’m sure the pharmaceutical reps are high-fiving right now.
Reginald Maarten
November 6, 2025 AT 08:11Actually, the 75% increased risk figure is misleading. It’s a relative risk increase, not absolute. The baseline risk of GI bleeding in healthy adults under 50 on both drugs is less than 0.5% annually. The increase pushes it to ~0.875%. That’s statistically significant, yes-but clinically, it’s still low for most. The real danger is in the elderly, those with prior ulcers, or on anticoagulants. Oversimplifying this as a universal catastrophe does more harm than good.
Bradley Mulliner
November 7, 2025 AT 07:29Of course the author is pushing PPIs. They’re profitable. They’re also overprescribed. Long-term PPI use increases risk of C. diff, bone loss, kidney disease, and micronutrient deficiencies. You’re trading one problem for three. And celecoxib? It’s a COX-2 inhibitor-linked to heart attacks. You want safer? Stop taking drugs altogether. Your body doesn’t need NSAIDs for mild pain. And SSRIs? They’re glorified placebos with side effects. Go meditate. Walk. Eat less sugar.
Jessica Adelle
November 7, 2025 AT 22:27It is profoundly irresponsible that such a preventable medical hazard continues to proliferate within the American healthcare apparatus. The failure of clinical protocols to mandate PPI co-prescription in this context reflects a systemic dereliction of duty. One does not simply prescribe two pharmacologically antagonistic agents without implementing protective measures-this is not medical practice; it is negligence dressed in jargon. The public must demand accountability.
Albert Schueller
November 8, 2025 AT 12:31Wait… so you’re telling me the FDA’s warnings aren’t enough? That doctors are just… ignoring them? And PPIs are the fix? Hmmm… I wonder if this is all part of a bigger scheme. Who owns the patent on omeprazole? Who profits from long-term prescriptions? Who controls the medical education curriculum? This isn’t about bleeding-it’s about control. The system wants you dependent on pills. Always pills. Never solutions.
Rahul hossain
November 10, 2025 AT 09:21My dear American friends, you have a beautiful obsession with pills-every ache, every sigh, every Tuesday blues, you reach for a capsule. In India, we have turmeric, ginger tea, yoga, and silence. We don’t need celecoxib or omeprazole. We need to stop treating symptoms and start living. Your stomach bleeds because you eat too much processed food, sit too long, and stress too hard. The drugs are just the symptom of a deeper sickness.
Sai Ahmed
November 10, 2025 AT 14:49They say NSAIDs and SSRIs cause bleeding. But what if it’s the other way around? What if the bleeding is caused by the government’s secret mind-control additives in tap water? I’ve read studies. The same labs that approved SSRIs also designed the fluoridation program. And PPIs? They’re just a distraction. They don’t fix the real problem-the neural dampeners in your coffee, your phone, your WiFi. You’re being poisoned. Slowly. Quietly. And they want you to take another pill.