Restless Legs and Iron: What Ferritin Levels Really Mean and How to Fix Them

If you’ve ever lain in bed at night feeling like your legs are crawling, tingling, or aching-with an irresistible urge to move them-you’re not alone. Restless Legs Syndrome (RLS), also called Willis-Ekbom Disease, affects 5-10% of adults in the U.S. and Europe. And while many assume it’s just stress or poor sleep, the real root cause for a large portion of these cases is something simple, measurable, and treatable: low iron in the brain.
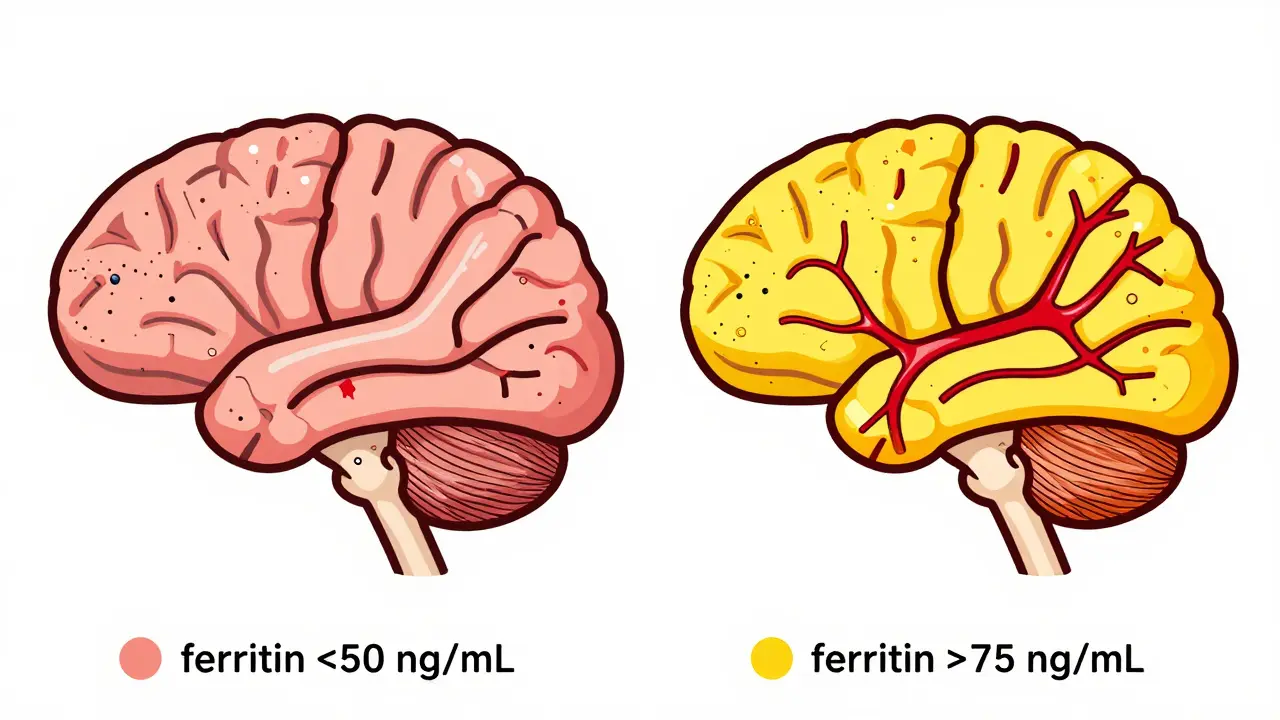
Here’s the twist: your blood test might say your iron is "normal." But that doesn’t mean your brain has enough. The key isn’t your serum iron-it’s your ferritin. And if your ferritin is below 50 ng/mL, you’re likely dealing with a treatable form of RLS.
Why Iron Matters More Than You Think
RLS isn’t just a muscle twitch or a nervous habit. It’s a neurological disorder tied to dopamine dysfunction in the brain. And dopamine needs iron to work properly. The substantia nigra, the part of your brain that produces dopamine, is especially sensitive to iron shortages. Even if your blood iron looks fine, your brain may be starving.
Studies show that people with RLS often have normal serum iron, but low ferritin-the storage form of iron that tells your body how much it has on hand. A 1997 study by Earley and colleagues found RLS patients had an average ferritin of 28.4 ng/mL, while healthy controls averaged 62.1 ng/mL. That gap hasn’t closed. In fact, more recent research confirms it: if your ferritin is under 50 ng/mL, you’re in the range where iron therapy can make a real difference.
This isn’t speculation. The American Academy of Neurology, the American Academy of Sleep Medicine, and the European Restless Legs Syndrome Study Group all agree: low ferritin is a key driver of RLS symptoms. And correcting it isn’t just helpful-it’s often the first step you should take before reaching for powerful medications.
The Magic Number: 50 ng/mL
Most labs list "normal" ferritin as 12-300 ng/mL. That’s a huge range. But for RLS, that range is misleading. You don’t need to be anemic to have RLS. You just need your brain iron to be too low.
The target isn’t 12 or even 30. It’s 50 ng/mL. That’s the threshold where symptoms start to improve in about half of patients. A 2020 study in Nature Scientific Reports showed that people with ferritin under 50 had worse symptoms and a higher risk of "augmentation"-a nasty side effect where RLS meds make symptoms spread to other body parts and get worse over time.
Even if your ferritin is between 50 and 75 ng/mL, you might still benefit. A 2019 study in the European Journal of Neurology found that 35% of patients in this "borderline" range saw symptom improvement after iron therapy. That’s why many sleep specialists now treat RLS based on ferritin, not just whether it’s "low" by lab standards.
Oral Iron: What Works (and What Doesn’t)
So how do you raise your ferritin? Most people start with oral iron supplements. The go-to is ferrous sulfate-325 mg tablets, which give you 65 mg of elemental iron. That’s a lot. And it’s usually taken on an empty stomach for best absorption.
But here’s the catch: up to 30% of people can’t tolerate it. Stomach pain, nausea, constipation-those are common. And if your gut doesn’t absorb well, the iron won’t reach your brain.
That’s why smart dosing matters. Instead of taking it daily, try every other day. A 2020 study in Blood Advances found that alternate-day dosing improved absorption and cut side effects by nearly half-without losing effectiveness. Pair your iron with 100-200 mg of vitamin C (like a glass of orange juice or a supplement). Vitamin C helps your body pull iron into your bloodstream.
Don’t take iron with calcium, antacids, or coffee. They block absorption. Wait at least two hours after eating if you’re taking it on an empty stomach.
And no, eating more spinach or red meat won’t fix this. A serving of steak gives you 1-2 mg of absorbable iron. You need 65 mg daily to make a dent in RLS. Supplements are necessary.
When Oral Iron Fails: IV Iron Is the Game-Changer
If you’ve tried oral iron for 8-12 weeks and your ferritin barely budged-or you couldn’t tolerate it-don’t give up. Intravenous (IV) iron is a powerful, underused tool.
The most common form used for RLS is ferric carboxymaltose. One single infusion of 1000 mg can boost ferritin by an average of 127 ng/mL within six weeks. That’s huge. A 2021 study in Sleep Medicine showed 68% of RLS patients had major symptom improvement after one IV dose.
And unlike oral iron, IV iron bypasses your gut entirely. No stomach issues. No absorption problems. Just direct delivery to your bloodstream.
It’s not perfect-it costs more, requires a clinic visit, and can cause temporary dizziness or flushing. But for people with ferritin under 30 ng/mL, or those who’ve failed oral therapy, it’s often the only thing that works.
And the effects last. A 2021 Neurology study followed patients for two years. Those who got IV iron maintained symptom control in 65% of cases. Compare that to 32% for people on long-term dopamine meds.
Why Dopamine Pills Aren’t the First Choice
Many doctors still start RLS patients on pramipexole or ropinirole. They work fast-sometimes in days. But they come with a dark side: augmentation.
Augmentation means your symptoms get worse. They start earlier in the day. Spread to your arms. Become more intense. Up to 80% of people on long-term dopamine therapy develop it. And once it happens, it’s hard to reverse.
Iron therapy doesn’t cause augmentation. Ever. It’s the only RLS treatment with that guarantee. And it targets the root cause, not just the symptoms.
The American Academy of Neurology gives iron therapy a "Level B" recommendation-"probably effective"-for patients with ferritin ≤ 75 ng/mL. That’s a strong endorsement. And sleep specialists surveyed in 2023 said 87% of them now prioritize iron repletion over dopamine drugs for patients with low ferritin.
What About Hepcidin? The Hidden Player
Why does iron get stuck in your gut and not reach your brain? The answer might be hepcidin. This hormone controls how much iron your body releases into the blood. In RLS patients, hepcidin levels are often too high-up to 12.4 ng/mL on average, compared to 8.1 ng/mL in healthy people.
High hepcidin = iron trapped in storage = brain starvation. That’s why some people with "normal" iron still have RLS.
Testing for hepcidin isn’t routine yet. But emerging research shows it’s a powerful predictor. A 2023 study found that patients with ferritin under 50 ng/mL and hepcidin over 10 ng/mL had a 78% chance of responding to iron therapy. Those with low hepcidin? Only 32% responded.
It’s not standard practice today-but it’s coming. In the next few years, hepcidin testing may become part of the RLS workup.

What to Do Next: Your Action Plan
If you have RLS, here’s what to do right now:
- Get your ferritin tested. Don’t rely on "normal" lab ranges. Ask specifically for the number.
- If it’s below 50 ng/mL: start oral iron. Take 65 mg elemental iron (one 325 mg ferrous sulfate tablet) every other day with vitamin C.
- If it’s between 50-75 ng/mL: consider a trial of iron anyway. Many people improve.
- If you can’t tolerate oral iron, or your ferritin stays under 30 ng/mL after 3 months: talk to your doctor about IV iron.
- Don’t start dopamine meds unless you’ve tried iron first. They’re not the answer-they’re the backup plan.
- Re-test ferritin after 8-12 weeks. Target: 75-100 ng/mL for best results.
Most people see improvement in 4-8 weeks. Some feel better sooner. Others need more time. But if you’re consistent, and your ferritin rises, your legs will thank you.
Cost, Safety, and Long-Term Gains
Oral iron costs $185-$350 a year. Dopamine meds? $2,400-$4,800. And that’s before side effects, doctor visits, or hospital trips for augmentation.
IV iron costs more upfront-$1,000-$2,000 per infusion-but you often only need one or two. And the payoff? Fewer medications, better sleep, no worsening symptoms, and a real shot at long-term control.
Iron therapy is safe when monitored. Too much iron can be dangerous-but that’s rare with proper testing. Your doctor will check ferritin and iron levels before and after treatment to make sure you’re not overdoing it.
This isn’t a miracle cure. But for the millions of people with RLS tied to low iron, it’s the closest thing we have to one.
What’s Next for RLS Treatment?
New iron formulations are on the horizon. Liposomal iron and ferric maltol are showing promise in early trials. They’re easier on the stomach, better absorbed, and may work faster.
The American Academy of Sleep Medicine is expected to update its guidelines in 2024 to recommend IV iron as a first-line option for patients with ferritin under 75 ng/mL. That’s a big shift-and it’s based on solid data.
One thing’s clear: iron isn’t just a supplement for RLS. It’s the foundation of treatment. And if you’ve been struggling with restless legs, you owe it to yourself to check your ferritin. It could change your sleep-and your life.

Manan Pandya
December 31, 2025 AT 07:47Finally, someone breaks down the ferritin-RLS link properly. I’ve been telling my neurologist for years that my serum iron was ‘normal’ but my legs still felt like they were full of ants at night. Ferritin at 22 ng/mL - started oral iron every other day with vitamin C. Six weeks later, symptoms cut by 70%. No dopamine meds needed. This is evidence-based, not guesswork.
Duncan Careless
December 31, 2025 AT 20:54Thank you for this. I’m a sleep tech in London and see so many patients on pramipexole who are clearly iron deficient. We don’t test ferritin routinely here - shame. I’ve started printing out this article and handing it to patients. If ferritin’s under 50, I push for iron first. It’s wild that guidelines haven’t caught up yet.
Nisha Marwaha
January 2, 2026 AT 13:10From a clinical neurology standpoint, the hepcidin angle is the real frontier. Elevated hepcidin in RLS isn’t just correlated - it’s mechanistically central. Iron absorption is gated by hepcidin-mediated ferroportin internalization. When hepcidin is chronically elevated - often due to low-grade inflammation or genetic polymorphisms in HFE - iron gets sequestered in enterocytes and macrophages. That’s why oral iron fails even when compliance is perfect. IV iron bypasses this entirely. The 2023 paper in JAMA Neurology showing hepcidin >10 ng/mL predicts 78% response to iron therapy? That’s practice-changing. We need point-of-care hepcidin assays. Now.
Nicole K.
January 3, 2026 AT 10:48So you’re saying I should just take iron pills instead of seeing a real doctor? That’s dangerous. What if you have hemochromatosis? People die from too much iron. This is irresponsible advice.
Alex Ronald
January 3, 2026 AT 22:22^ This is why I love this community. You’re right to be cautious, but the key is monitoring. Ferritin under 50 = safe to supplement. Re-test after 3 months. No one’s suggesting mega-doses. And hemochromatosis is rare - about 1 in 200 of Northern European descent. Most people with RLS are just iron-starved brains, not iron-overloaded. This isn’t guesswork - it’s protocol.
Marie-Pierre Gonzalez
January 4, 2026 AT 18:41I’m so grateful for this post. I’ve suffered for 12 years. Thought it was ‘anxiety.’ Took ferrous sulfate for 6 weeks - couldn’t handle the nausea. Switched to ferrous bisglycinate (gentler on stomach) + 200mg vitamin C every other day. Ferritin went from 31 to 89 in 10 weeks. No more midnight leg screaming. 🙏 I’m finally sleeping.
Himanshu Singh
January 5, 2026 AT 09:17Bro, I tried everything - yoga, magnesium, warm baths. Nothing worked. Then I checked my ferritin - 28. Started iron every other day. Two weeks later, I slept through the night for the first time in years. I’m not even kidding. This changed my life. Thank you for sharing the science!
Amy Cannon
January 5, 2026 AT 10:59As someone who has spent the last decade navigating the labyrinthine world of chronic neurological dysfunction, I must emphasize that the paradigm shift toward ferritin-centric management of Restless Legs Syndrome represents not merely a clinical adjustment but a fundamental reorientation of therapeutic priorities within sleep medicine. The persistence of dopamine agonist-first protocols, despite overwhelming evidence of augmentation risk and the non-inferiority - indeed, superiority - of iron repletion in low-ferritin populations, reflects a troubling inertia within medical education and institutional guidelines. The data from the European RLS Study Group, the AAN, and the 2021 Sleep Medicine meta-analysis collectively compel a revision of standard-of-care algorithms. Moreover, the emerging role of hepcidin as a regulatory biomarker suggests that future diagnostic workflows must integrate inflammatory and iron-metabolic profiling, moving beyond the reductive paradigm of serum iron alone. We are, quite literally, at the dawn of a new era in RLS therapeutics - one where treating the brain’s iron deficit, not masking its dopamine dysfunction, becomes the cornerstone of intervention.
Teresa Rodriguez leon
January 7, 2026 AT 05:54I’ve been on ropinirole for 5 years. Augmentation hit me hard. Now my arms twitch too. I tried iron but it made me constipated and I felt worse. I don’t trust this ‘iron cure’ hype. You’re just pushing supplements because you hate pharma.
Paige Shipe
January 7, 2026 AT 12:48You’re not listening. I tried iron. It didn’t work. I have the science. I’ve read the papers. You’re all just giving people false hope. I’ve been on dopamine meds for 7 years. I know what works. And it’s not iron.