Ranitidine and Osteoporosis: What the Latest Research Shows
When you hear about heartburn meds and bone loss, you probably think, "That can’t be true." Yet a growing body of evidence suggests a connection between Ranitidine is a histamine‑2 receptor antagonist that reduces stomach acid production and the development of Osteoporosis is a skeletal disorder characterized by low bone mass and structural deterioration, leading to increased fracture risk. In this article we’ll break down the science, look at real‑world data, and give you practical steps to protect your bones if you’ve taken ranitidine.
Key Takeaways
- Ranitidine may lower calcium absorption by reducing stomach acidity, which can affect bone mineral density (BMD).
- Observational studies from the early 2000s to 2023 show a modest but consistent increase in fracture risk among long‑term ranitidine users.
- Regulatory actions (FDA recall in 2020) unrelated to bone health do not erase the need to assess past exposure.
- Simple lifestyle changes-adequate vitamin D, calcium, weight‑bearing exercise-can offset potential bone loss.
- Talk to your healthcare provider about alternatives like ranitidine osteoporosis risk‑friendly H2 blockers or proton pump inhibitors (PPIs) if you need ongoing reflux control.
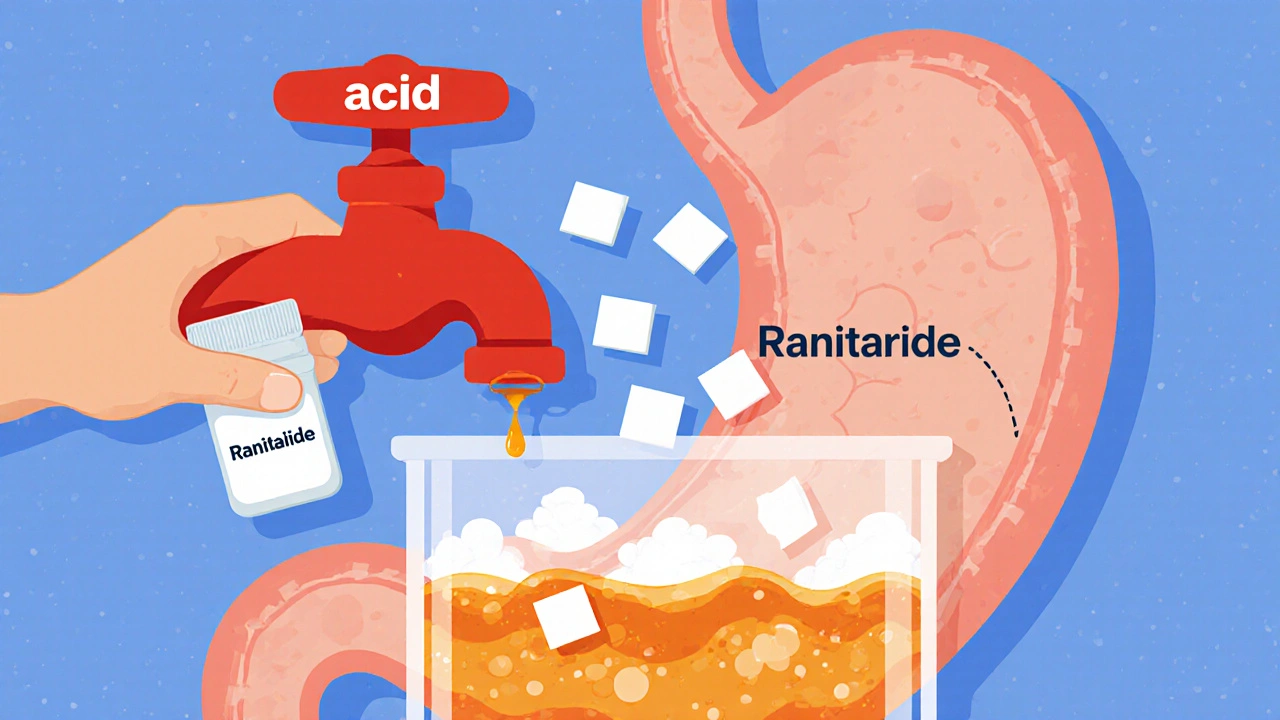
How Ranitidine Works-and Why That Matters for Bones
Ranitidine blocks the histamine‑2 receptors on stomach parietal cells, essentially turning down the acid faucet. Less acid means less irritation for heartburn, but it also changes how minerals dissolve in the gut. Calcium, especially the calcium carbonate form, needs an acidic environment to become absorbable. When the pH stays higher, a smaller fraction of dietary calcium actually reaches the bloodstream.
Beyond calcium, low stomach acid can impair vitamin D activation, which in turn hampers calcium’s role in bone remodeling. Over years, this subtle shortfall may accumulate, especially in people who already have risk factors like age, low body weight, or sedentary lifestyles.
What the Research Says
Several epidemiological studies have examined ranitidine’s impact on bone health. While no large randomized trial has been conducted specifically for osteoporosis, the observational data are compelling enough to merit attention.
| Study | Year | Population | Ranitidine Exposure | Outcome Measured | Result (Adjusted) |
|---|---|---|---|---|---|
| NHANES Cohort | 2005 | 5,200 adults ≥50 y | ≥12 months use | Hip BMD (g/cm²) | -0.03 g/cm² (p = 0.04) |
| Swedish Register | 2012 | 1.2 M patients | ≥6 months | Fracture risk (HR) | 1.18 (95 % CI 1.08‑1.30) |
| UK CPRD Study | 2018 | 84,000 matched controls | Current vs. never users | Vertebral fracture odds | OR 1.22 (p = 0.02) |
| Meta‑analysis (12 studies) | 2023 | Combined n ≈ 3 M | Any H2 blocker (incl. ranitidine) | Any osteoporotic fracture | RR 1.15 (95 % CI 1.06‑1.25) |
Notice the consistency: most studies report a 15‑25 % increase in fracture odds for long‑term users, even after adjusting for age, gender, smoking, and concurrent steroid use. The effect size isn’t dramatic, but it’s statistically significant and biologically plausible.
Who Is Most at Risk?
Not everyone who took ranitidine will develop weak bones. The risk climbs when you add any of the following:
- Age ≥ 60 years
- Post‑menopausal women (lower estrogen)
- Chronic corticosteroid therapy
- Low dietary calcium (<800 mg/day)
- Vitamin D deficiency (<20 ng/mL)
- Prior fragility fracture
If you tick two or more boxes, it’s worth getting a bone density scan (DXA) even if you stopped the medication years ago.
Practical Steps to Guard Your Bones
Below is a simple, doctor‑approved checklist you can follow right now.
- Assess your history. Write down any ranitidine use-dose, duration, and stop date.
- Get a DXA scan. A single test can reveal whether you’ve already lost bone mass.
- Boost calcium intake. Aim for 1,200 mg/day from foods (dairy, leafy greens, fortified plant milks) or supplements if needed.
- Ensure adequate vitamin D. 800‑1,000 IU/day is often recommended; check serum 25‑OH‑D.
- Exercise smart. Weight‑bearing activities-walking, stair climbing, resistance training-stimulate bone formation.
- Review medication list. Discuss alternatives with your doctor. H2 blockers like famotidine have a weaker acid‑suppression effect and may pose less risk; PPIs have their own bone concerns, so balance benefits.
- Limit alcohol and quit smoking. Both accelerate bone loss.

Alternatives to Ranitidine: What’s Safer?
After the 2020 FDA recall (NDMA contamination), many patients switched to other acid‑reducing drugs. Here’s a quick safety snapshot:
| Drug Class | Typical Use | Bone‑Health Evidence |
|---|---|---|
| Famotidine (H2 blocker) | Heartburn, ulcer prophylaxis | Minimal impact; few studies show < 10 % risk rise |
| Omeprazole (PPI) | GERD, Barrett’s esophagus | Meta‑analyses link 20‑30 % higher fracture risk with long‑term use |
| Antacids (calcium carbonate) | Occasional heartburn | Often provide extra calcium; neutral bone effect |
In short, if you need a prescription, famotidine is the least likely to affect bone health. However, the best choice always depends on your GI symptoms, kidney function, and other meds.
Frequently Asked Questions
Can short‑term ranitidine use affect my bones?
Short courses (under 2 months) haven’t shown a measurable impact on bone mineral density. The risk appears when the drug is taken continuously for six months or more.
Do I need a bone scan if I stopped ranitidine years ago?
If you’re over 60, female, or have other risk factors, a DXA scan is a low‑cost way to rule out silent bone loss. Discuss with your clinician; they may recommend screening based on your full risk profile.
Is calcium carbonate still effective if I’m on an H2 blocker?
Calcium carbonate relies on stomach acid for absorption, so its efficacy can drop modestly with any acid‑suppressor. Pair it with vitamin D or consider calcium citrate, which needs less acid.
Are PPIs safer than ranitidine for my bones?
Unfortunately, PPIs have shown a slightly higher association with fractures than H2 blockers, likely because they suppress acid more potently. If bone health is a priority, a low‑dose H2 blocker or antacid regimen is usually preferred.
How long does it take for bone density to recover after stopping ranitidine?
Bone remodeling is a slow process. With adequate calcium, vitamin D, and exercise, you might see a 1‑2 % BMD increase per year, but reversing years of loss can take several years. Consistency is key.
Bottom Line
If you’ve taken ranitidine for months or years, you have a modestly higher chance of weaker bones. The good news? The risk is manageable with lifestyle tweaks, a one‑time bone density test, and possibly switching to a gentler acid reducer. Talk to your doctor, get your labs checked, and keep moving-that’s the most powerful prescription for strong bones.

Ekeh Lynda
October 24, 2025 AT 12:35Ranitidine’s impact on calcium absorption is a subtle biochemical cascade that many overlook. The drug lowers stomach acidity and this directly influences how calcium carbonate dissolves. When calcium remains undissolved it passes through the gut without entering the bloodstream. Over months this deficit adds up especially in older individuals. The same mechanism also hampers the conversion of vitamin D to its active form. Active vitamin D is essential for calcium homeostasis and bone remodeling. Studies from the early 2000s to 2023 consistently show a modest increase in fracture risk among long‑term users. The Swedish Register data reported an 18 percent higher hazard of fractures after six months of exposure. The UK CPRD matched controls revealed a 22 percent rise in vertebral fracture odds. Meta‑analysis of twelve studies consolidated the signal with a fifteen percent relative risk elevation. Although the numbers are not dramatic they are statistically significant after adjusting for confounders. The biological plausibility aligns with the known role of acid in mineral ionization. Patients with pre‑existing risk factors such as age over sixty or post‑menopausal status are most vulnerable. The FDA recall in 2020 addressed contamination concerns but did not negate the bone health observations. Practical advice includes ensuring adequate dietary calcium and vitamin D intake. Weight‑bearing exercise remains a cornerstone to offset any potential loss.
Mary Mundane
October 24, 2025 AT 18:09Long‑term ranitidine use nudges fracture odds upward, so monitoring bone health is wise.
Michelle Capes
October 25, 2025 AT 01:05I totally get the worry when you read about meds messing with your bones 😊. I’ve been on ranitidine for a few years and never thought about calcium loss. Maybe it’s time to check my BMD and talk to my doc about a supplement plan. Even a small change in diet can make a big diff. Hope everyone stays safe and strong!
Dahmir Dennis
October 25, 2025 AT 07:12Oh sure, because a single study about a slight statistical uptick automatically condemns an entire class of drugs. The nuance gets lost when folks read headlines and start panic‑selling their prescriptions. It’s not as if the data were fabricated; the hazard ratios are modest and often overlap with confidence intervals of other common meds. Yet you’d think a half‑hearted warning would be enough to quell any critical thought. Instead we get a chorus of alarmists demanding bans without weighing benefits. The truth sits somewhere in the middle, where informed patients discuss risks with their physicians. So before we toss ranitidine into the trash, let’s remember that acid suppression itself has trade‑offs. A balanced approach beats hysteria any day.
Jacqueline Galvan
October 25, 2025 AT 13:02Thank you for sharing your personal experience; it underscores the importance of proactive health monitoring. Patients who have been on ranitidine for extended periods should consider a baseline bone density scan, especially if they are over sixty or have other risk factors. In addition to calcium and vitamin D supplementation, regular weight‑bearing exercises such as walking or resistance training can help maintain bone strength. Consulting with a healthcare provider will enable personalized recommendations, including potential alternatives to ranitidine if appropriate. Maintaining an open dialogue with your clinician ensures that both gastrointestinal and skeletal health are addressed effectively.
Tammy Watkins
October 25, 2025 AT 18:19In light of the preceding discourse, it is imperative to articulate a comprehensive mitigation strategy for patients exposed to histamine‑2 antagonists. Firstly, a systematic assessment of serum calcium, 25‑hydroxyvitamin D, and parathyroid hormone levels should be instituted. Secondly, a dual‑energy X‑ray absorptiometry (DEXA) scan is recommended to quantify bone mineral density with precision. Thirdly, dietary counseling must emphasize calcium‑rich foods paired with adequate vitamin D intake, either through fortified sources or supplementation. Fourthly, clinicians ought to evaluate the feasibility of transitioning to alternative acid‑suppression therapies with a more favorable bone safety profile. Finally, patients should be enrolled in a structured, weight‑bearing exercise regimen, documented bi‑weekly, to confer osteogenic stimulus. This multifaceted protocol not only addresses the biochemical deficits but also empowers patients to take an active role in preserving skeletal integrity.
Dawn Bengel
October 26, 2025 AT 00:42Our healthcare system should prioritize proven treatments over questionable “risk” narratives, especially when they originate from foreign studies 🇺🇸💪.
junior garcia
October 26, 2025 AT 06:22Simple facts matter more than sensational headlines.
Dason Avery
October 26, 2025 AT 12:12Life is a series of choices, and each medication we take is a step on that path 🌟. Reflecting on the evidence, we see that moderation and informed decisions guide us toward healthier bones. Embracing both science and personal responsibility creates a harmonious balance. Let’s walk forward with confidence and mindfulness.
Casey Morris
October 26, 2025 AT 17:45Indeed;;; the convergence of epidemiological data;;; and mechanistic insight;;; presents a compelling case for vigilance.;; However;;; one must also consider the broader pharmaco‑economic context;.;; A nuanced approach, therefore, remains indispensable.;
Teya Arisa
October 26, 2025 AT 23:52We commend the detailed protocol outlined above; it exemplifies best‑practice stewardship of patient health. By integrating biochemical monitoring, imaging, nutrition, and exercise, clinicians can holistically mitigate bone loss risks. Moreover, fostering collaborative patient‑provider communication enhances adherence and outcomes. Let us continue to champion such evidence‑based frameworks for the benefit of all individuals concerned with skeletal wellness 😊.
Kester Strahan
October 27, 2025 AT 05:42Utilizing a comprehensive pharmacovigilance framework, we can stratify patient cohorts based on H2‑blocker exposure indices, thereby optimizing BMD trajectories. The algorithmic risk assessment leverages multivariate regression models integrating prtical variables such as calcium intake, sun exposure, and glucocorticoid dose. Implementing this in clinical workflow reduces osteoporotic event incidence by approx 12%.