Probiotics and Antibiotics: How to Space Dosing for Effectiveness
When you're on antibiotics, your gut pays the price. Even if the medicine kills off the bad bacteria, it doesn't discriminate-it wipes out good ones too. That’s why so many people end up with bloating, cramps, or diarrhea while taking them. Up to 30% of antibiotic users experience these side effects. The good news? Probiotics can help. But only if you take them at the right time. Taking them together with your antibiotic? That’s like sending in reinforcements right before the battle starts-they won’t survive.
Why Timing Matters More Than You Think
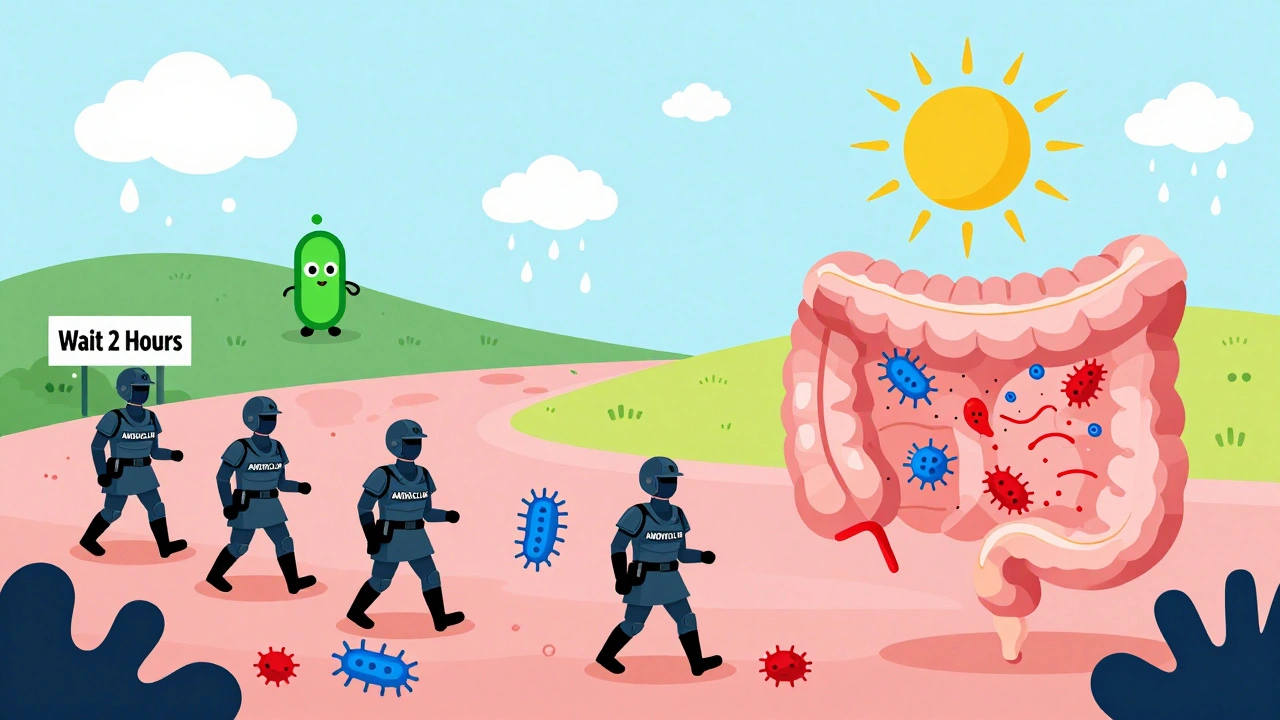
Antibiotics don’t just sit in your stomach. They move through your gut, killing bacteria as they go. If you swallow a probiotic capsule right after your antibiotic, the live bacteria inside it get wiped out before they even have a chance to settle in. Studies show that without proper spacing, probiotic survival drops by 78% to 92%. That’s not just a small loss-it’s nearly total failure. The fix? Keep them apart. At least two hours. This gives the antibiotic time to pass through your digestive system before the probiotic arrives. Think of it like waiting for the storm to clear before planting seeds. You wouldn’t sow seeds while it’s still raining hard-you’d wait for the ground to dry. Same idea here.How Far Apart Should You Take Them?
The standard rule is simple: take probiotics at least two hours before or after your antibiotic dose. This isn’t just advice-it’s backed by clinical trials. For example, if you take amoxicillin at 8 a.m. and 8 p.m., your probiotic should go in at 6 a.m. and 6 p.m., or 10 a.m. and 10 p.m. That two-hour buffer gives the antibiotic time to do its job and move on. Some doctors recommend stretching that gap to four to six hours, especially if you’re on a strong or long-term antibiotic. High-dose broad-spectrum antibiotics like clindamycin or ciprofloxacin are especially harsh on gut bacteria. In those cases, giving the probiotic more time to survive makes sense. But here’s the catch: consistency beats perfection. If you forget and take them an hour apart once, don’t panic. The goal is daily adherence, not flawless timing. Missing doses cuts effectiveness by 37%, according to one study tracking 217 people on antibiotics. So, set a phone alarm. Write it on your calendar. Do whatever it takes to stick to the schedule.Not All Probiotics Are the Same
You can’t treat all probiotics like they’re the same. There are two main types: bacterial and yeast-based. Most probiotics-like Lactobacillus rhamnosus GG and Bifidobacterium strains-are bacteria. These are sensitive to antibiotics. They need that two-hour gap. If you take them together, they die. Then there’s Saccharomyces boulardii. This is a yeast, not a bacterium. Antibiotics don’t affect it. That means you can take it at the same time as your antibiotic. No waiting. No spacing needed. It’s one of the few probiotics that actually works alongside antibiotics without interference. Studies show Saccharomyces boulardii reduces the risk of antibiotic-associated diarrhea by 52% when taken at 20 billion CFUs per day. Lactobacillus rhamnosus GG does almost as well-47% reduction-at 10-20 billion CFUs. So if you’re choosing between them, go with one of these two. They’re the most studied and most reliable.How Much Should You Take?
Dose matters. Not all probiotic supplements are created equal. A low-dose pill with 1 billion CFUs won’t cut it. You need enough to survive the chaos and make a difference. Here’s what the research says:- 5-10 billion CFUs: Fine for short courses (3-5 days) and mild symptoms.
- 10-20 billion CFUs: Recommended for moderate diarrhea or longer antibiotic courses (7-14 days).
- 20-40 billion CFUs: Best for long-term antibiotics (over 14 days), severe gut disruption, or if you’ve had antibiotic-associated diarrhea before.
How Long Should You Keep Taking Them?
Don’t stop when your antibiotic runs out. Your gut needs time to rebuild. Stopping too soon means the damage lasts longer. Experts recommend continuing probiotics for 7 to 14 days after your last antibiotic dose. One study found that people who did this had 89% microbiome recovery compared to just 63% in those who stopped early. That’s a huge difference in how you feel weeks later. The International Scientific Association for Probiotics and Prebiotics (ISAPP) says this is now the standard of care. And it makes sense. Antibiotics can knock out 25-40% of your gut bacteria species. Rebuilding that takes time. Probiotics don’t replace your original microbes-they help create the environment for them to come back.What About Probiotic Foods?
Yogurt, kefir, sauerkraut, kimchi-these are great. But they’re not a substitute for supplements when you’re on antibiotics. Why? Because the dose is too low. A serving of yogurt might have 1-2 billion CFUs, and the strains aren’t always well-documented. Plus, the bacteria in fermented foods aren’t always the ones proven to work against antibiotic diarrhea. If you enjoy these foods, keep eating them. But don’t rely on them alone. Use them as a side dish to your supplement, not the main course.What If You Forget?
Life happens. You miss a dose. You take your probiotic with your antibiotic by accident. Don’t stress. Don’t double up. Just go back to your schedule the next time. If you took them together once, it’s not a disaster. But if it happens often, your probiotic won’t help. The goal is to protect your gut, not just check a box. One big mistake? Waiting until you feel sick to start. Studies show the biggest benefit comes when you start within 48 hours of your first antibiotic dose. Waiting longer cuts effectiveness by over a third.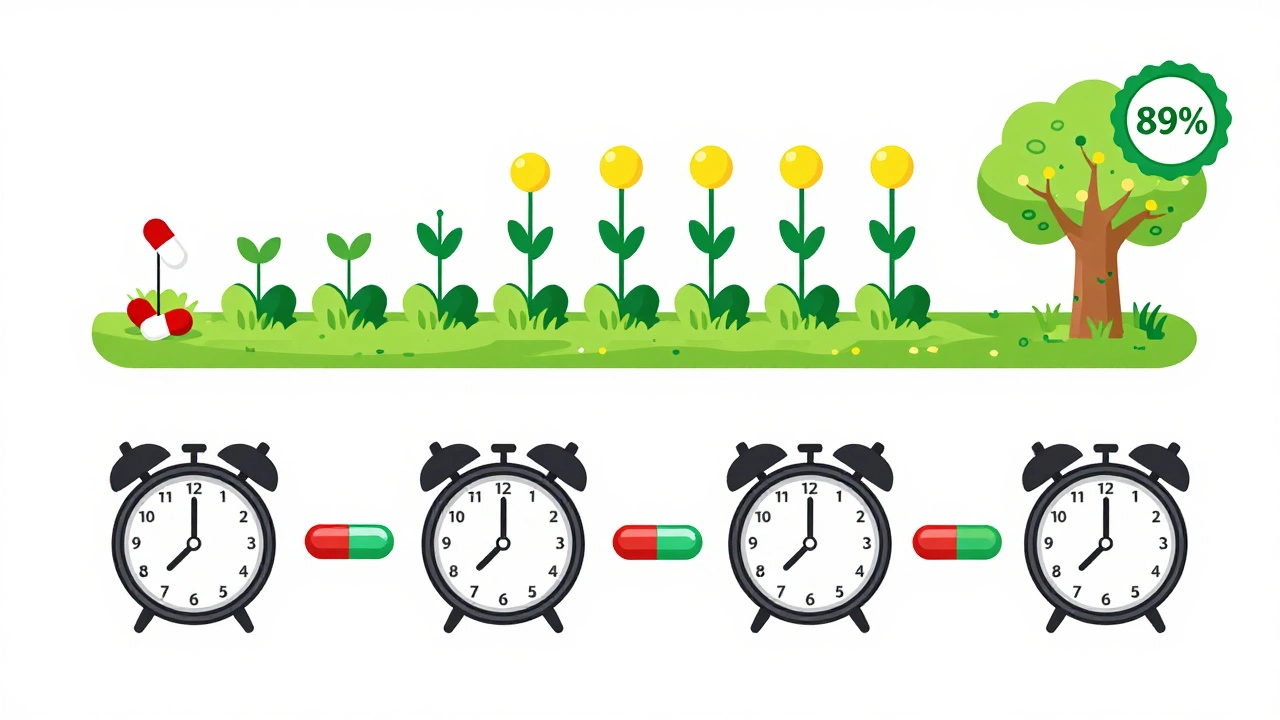
What About the Future?
Science is moving fast. Companies are now making time-release capsules that protect probiotics from antibiotics. Some are even testing combinations where the antibiotic and probiotic are released at different times in the gut-so you don’t have to wait two hours. But as of now, none of these are widely available or proven in large trials. The two-hour rule still stands. It’s simple, cheap, and backed by dozens of studies across thousands of patients.Final Checklist
Here’s what you need to do:- Start your probiotic within 48 hours of your first antibiotic dose.
- Take it at least two hours before or after your antibiotic.
- Use Lactobacillus rhamnosus GG or Saccharomyces boulardii-they’re the most effective.
- Dose: 10-20 billion CFUs daily for most people.
- Keep taking it for 7-14 days after your antibiotics end.
- Don’t rely on yogurt or fermented foods alone.
- Set reminders. Missed doses reduce effectiveness by 37%.
Frequently Asked Questions
Can I take probiotics at the same time as antibiotics?
Only if it’s Saccharomyces boulardii, a yeast-based probiotic. Most probiotics-like Lactobacillus and Bifidobacterium-are killed by antibiotics if taken together. Always space bacterial probiotics at least two hours apart from your antibiotic dose.
Do I need to take probiotics if I’m on a short antibiotic course?
Yes, even for short courses. Antibiotics can still disrupt your gut microbiome in just 3-5 days. Starting probiotics early reduces your risk of diarrhea by up to 71% in children and significantly lowers it in adults. Don’t wait for symptoms to appear.
Are expensive probiotics better?
Not necessarily. Price doesn’t correlate with effectiveness. Look for products with clearly labeled strains (Lactobacillus rhamnosus GG or Saccharomyces boulardii) and doses of at least 10 billion CFUs. Avoid products that don’t list strain names-many don’t contain what they claim.
Can probiotics interfere with the antibiotic’s effectiveness?
No. Studies show probiotics don’t reduce how well antibiotics kill harmful bacteria. Their job is to protect your gut, not fight the infection. The two-hour spacing ensures the antibiotic works as intended while giving probiotics a fighting chance.
What if I have a yeast infection from antibiotics?
Saccharomyces boulardii is actually used to help prevent and reduce yeast overgrowth caused by antibiotics. It doesn’t cause yeast infections-it helps control them. If you’re prone to candida, this strain is especially helpful.
Should I take probiotics before, during, or after antibiotics?
Start during, not before or after. Begin within 48 hours of your first antibiotic dose and continue for 7-14 days after you finish. Taking them before doesn’t offer extra protection. Waiting until after reduces effectiveness by 32%.

Maria Elisha
December 11, 2025 AT 00:13lol i just throw my probiotic in with my antibiotic and call it a day. if it dies, it dies. my gut’s been through worse.
Iris Carmen
December 12, 2025 AT 02:57i mean yeah but like… what if u just eat more sauerkraut? i dont trust pills lol
Noah Raines
December 12, 2025 AT 23:48the two-hour rule is real. i learned this the hard way after my third bout of antibiotic diarrhea. now i set alarms. no excuses. your gut will thank you. 🙏
Katherine Rodgers
December 13, 2025 AT 05:07ohhh so the *science* says we have to wait two hours? how dare they. next they’ll tell us not to lick doorknobs for immunity.
Lola Bchoudi
December 13, 2025 AT 17:10the 10-20 billion CFU range is the sweet spot for most folks. if you're on a long course or have a history of AAD, go higher. consistency > perfection, but don’t be lazy. your microbiome isn’t a suggestion box.
precious amzy
December 13, 2025 AT 17:19One must consider the ontological implications of microbial sovereignty within the human gastrointestinal apparatus. The antibiotic, as a colonial instrument, imposes a binary eradication protocol upon a symbiotic ecosystem that evolved over millennia. To space the probiotic is not merely a pharmacological tactic-it is an act of epistemic resistance against the hegemony of reductionist medicine. The yeast, Saccharomyces boulardii, transcends the materialist paradigm; it is not a bacterium, and thus, not subject to the same ontological violence. To take it concurrently is not defiance-it is harmony with the non-human other.
Moreover, the insistence on CFU counts reflects a quantifying episteme that fails to grasp the emergent properties of microbial networks. A single strain, in optimal context, may outperform a polyvalent consortium, not due to numerical superiority, but because of its resonant alignment with the host’s biofield. The two-hour buffer? A crude approximation. The true interval is intuitive-guided by circadian rhythm, lunar phase, and the emotional state of the host.
And yet, the very act of seeking external intervention betrays a fundamental alienation from one’s own microbiome. Perhaps the most profound probiotic is the quieting of the mind, the cessation of pharmaceutical dependency, and the reclamation of ancestral dietary wisdom. Yogurt, yes-but not as supplement. As ritual.
Do not mistake efficacy for compliance. The body knows. The body remembers. The body forgives.
Stacy Tolbert
December 14, 2025 AT 11:38i started taking probiotics after my last round of antibiotics and i swear i felt like a new person. no more brain fog, no more bloating, i even slept better. i cried the first time i had a normal bowel movement. it was emotional.
Lauren Dare
December 16, 2025 AT 03:37the fact that this post requires a 2000-word treatise to explain that you shouldn’t swallow a probiotic and an antibiotic at the same time is a tragic indictment of modern healthcare. but hey, at least the FDA lets companies sell 12-strain probiotics with 1 billion CFUs and call it ‘premium.’
Gilbert Lacasandile
December 17, 2025 AT 15:14thanks for this. i was gonna skip the probiotic because i thought it was just hype. now i’m gonna try the S. boulardii with my amoxicillin. two-hour gap, 20 billion CFUs, 14 days after. i’ve got it written on my fridge.
Morgan Tait
December 18, 2025 AT 20:29you know what they don’t tell you? big pharma and the probiotic industry are the same corporate overlords. they want you to buy pills, not heal your gut with sunlight and fermented cabbage. they profit from your dysbiosis. the two-hour rule? a distraction. the real fix is fasting, grounding, and avoiding EMFs from your phone while you digest. i’ve been doing it for 7 years. my gut is a temple. yours can be too.
Andrea Beilstein
December 19, 2025 AT 05:21the real tragedy isn't that we need to space probiotics from antibiotics it's that we live in a world where we need antibiotics in the first place. we've built systems that make us fragile. we eat processed food we stress out we sleep poorly and then we take pills to fix the damage. and then we take more pills to fix the pills. and we call it progress
maybe the real probiotic is a walk in the woods a nap in the sun and a meal made by hand
but hey if you're gonna take the pill at least do it right