Link Between Upset Stomach and Migraines - What You Need to Know

Gut-Brain Symptom Tracker
Log your daily symptoms to track patterns between stomach discomfort and headaches. This tool helps identify potential triggers in your gut-brain axis.
Recent Entries
TL;DR
- Stomach discomfort can fire up migraine attacks through the gut‑brain axis.
- Key culprits include food intolerances, low serotonin, dehydration and stress.
- Keeping a symptom diary helps pinpoint personal triggers.
- Simple diet tweaks, hydration habits and stress‑relief techniques often reduce both stomach pain and head pain.
- Seek medical advice if attacks become frequent or severe.
Ever notice that a bout of stomach cramps seems to be followed by a pounding headache? You’re not imagining it. Scientists increasingly see the digestive system and the brain as conversation partners, and when the gut gets upset, the brain can fire off a migraine. This article unpacks why an upset stomach and a migraine often travel together, what biology lies underneath, and practical steps you can take to break the cycle.
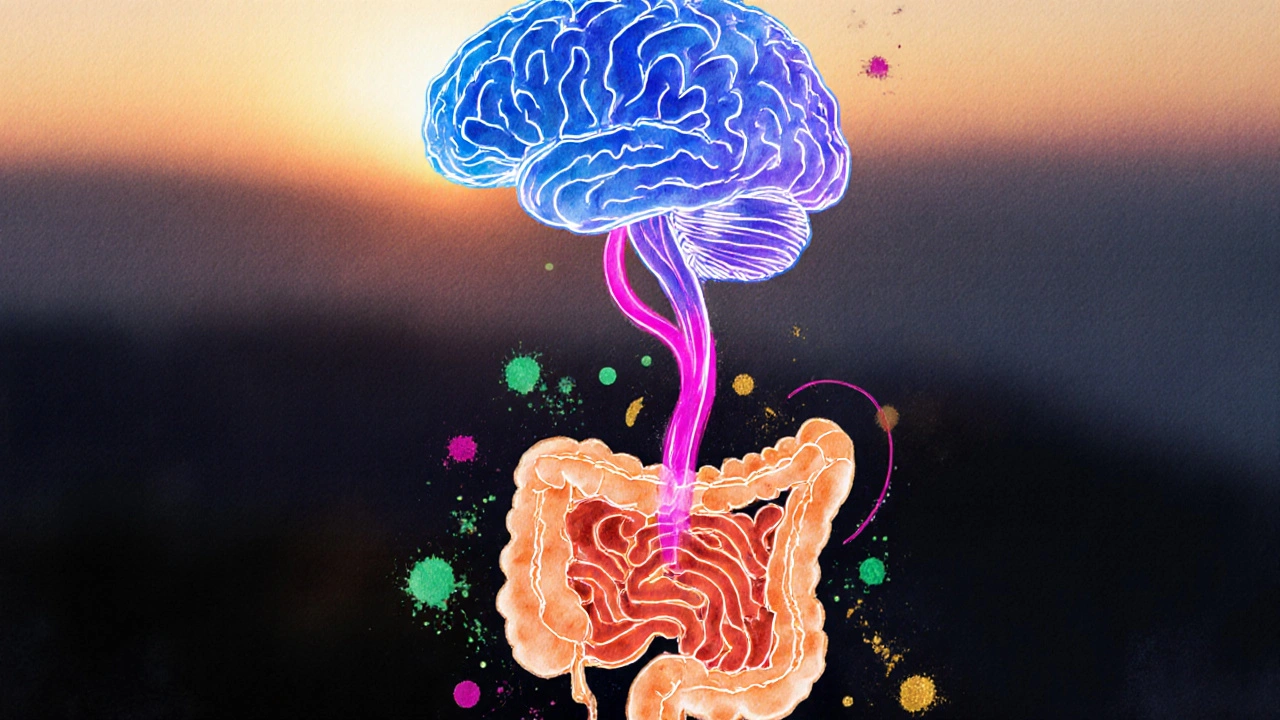
How the Gut‑Brain Axis Works
Gut‑brain axis is a two‑way communication network that links the gastrointestinal tract with the central nervous system. It uses neural pathways, hormones and immune signals to keep everything in sync. When the gut sends a distress signal-like inflammation or an imbalance of microbes-the brain can interpret that as pain, nausea or, in some people, a migraine.
Common Stomach Issues That Spark Headaches
Upset stomach covers a range of symptoms: bloating, cramping, diarrhea, and acid reflux. Below are the most frequent offenders that tend to overlap with migraine episodes.
- Food intolerances - Lactose, gluten or certain additives can irritate the gut lining and trigger inflammatory cascades.
- Low stomach acid - Poor digestion leads to fermentation, gas buildup and pressure on the vagus nerve.
- Dehydration - Not drinking enough water makes stools hard, reduces blood volume, and can provoke both abdominal pain and vascular headaches.
- Stress‑related gut motility changes - Anxiety can slow or speed up transit time, creating discomfort that the brain registers as a headache.
Physiological Pathways Connecting Digestion and Pain
Several mechanisms explain the stomach‑migraine link.
- Serotonin is a neurotransmitter made mostly in the gut. When the intestine is irritated, serotonin release spikes, sending signals that overstimulate the trigeminovascular system, the pain‑processing network behind migraines.
- Inflammatory cytokines from an upset gut travel through the bloodstream, lowering the threshold for neuronal firing in the brain.
- The vagus nerve, a major highway between belly and brain, can convey pain signals directly to the brainstem, where migraine generators reside.
- Changes in gut microbiota affect the production of short‑chain fatty acids, which modulate brain inflammation and pain perception.
Practical Steps to Break the Cycle
Below is a checklist you can start using today. It’s a blend of diet tweaks, hydration habits and lifestyle adjustments proven to calm both the gut and the head.
- Track symptoms: Write down every meal, beverage, stress event, stomach sensation and headache. After two weeks you’ll often see a pattern.
- Eliminate common triggers: Try a low‑FODMAP diet for three weeks, or cut out dairy and gluten one at a time to see if headaches improve.
- Stay hydrated: Aim for at least 2L of water daily. Add electrolytes if you sweat heavily.
- Mindful eating: Chew slowly, avoid large meals, and limit caffeine and alcohol, which can irritate the gut lining.
- Support gut health: Probiotic‑rich foods (yogurt, kefir, sauerkraut) or a quality supplement can rebalance microbiota.
- Stress management: Simple breathing exercises, short walks, or a 10‑minute meditation can keep the vagus nerve calm.
If you’re battling a migraine, the link to your upset stomach matters. Addressing the gut often reduces the frequency and severity of head pain without relying on extra medication.
When to Seek Professional Help
While many people can manage the connection at home, certain red flags call for a doctor’s expertise.
- Headaches that last longer than 72hours or worsen despite over‑the‑counter treatment.
- Sudden, severe abdominal pain with vomiting, fever or blood in stool.
- Weight loss, anemia or chronic diarrhea lasting more than a month.
- Family history of celiac disease, inflammatory bowel disease or severe migraine disorders.
Healthcare providers may order blood panels, stool tests or imaging studies to rule out underlying conditions. They can also recommend prescription‑level migraine preventives that target serotonin pathways, which may double‑duty for gut relief.
Quick Comparison of Common Triggers
| Trigger Type | Typical Symptoms | Impact on Gut‑Brain Axis |
|---|---|---|
| Food Intolerance (e.g., gluten) | Bloating, gas, cramping | Elevated gut inflammation → serotonin surge |
| Dehydration | Dry mouth, dark urine, constipation | Reduced blood volume → vascular constriction in brain |
| Sleep Deprivation | Fatigue, irritability | Alters cortisol, heightens vagal sensitivity |
| Hormonal Fluctuations | Mood swings, bloating | Modulates serotonin receptors in both gut and brain |
Bottom Line
The stomach‑migraine connection isn’t a myth; it’s a biologically wired dialogue that can go awry. By paying attention to what you eat, how you hydrate, and how you manage stress, you give both your gut and your brain a chance to breathe. If the problem persists, a clinician can dig deeper, test for hidden intolerances, and prescribe targeted therapies that calm the entire gut‑brain network.
Frequently Asked Questions
Can a single episode of food poisoning cause a migraine?
Yes. Acute gut inflammation releases cytokines and serotonin, which can briefly lower the headache threshold. Most people notice the pain subside once the stomach settles, but repeated exposure can build a pattern.
Is there a reliable test to confirm a gut‑related migraine?
No single test definitively links the two, but doctors often use a combination of food‑challenge trials, stool analysis for dysbiosis, and blood markers for inflammation. Correlating symptom diaries with test results helps build a convincing case.
Do probiotic supplements actually reduce migraine frequency?
Research shows certain strains (e.g., Lactobacillus rhamnosus) can modulate serotonin production and lower gut inflammation, which in turn may cut migraine days by 20‑30% for some users. Results vary, so trial and monitoring are key.
How much water should I drink to prevent both stomach pain and headaches?
Aiming for about 2liters (8 cups) daily works for most adults, but increase intake if you exercise, live in a hot climate, or notice dark urine. Adding a pinch of salt or an electrolyte tablet can help retain fluid.
When should I consider seeing a neurologist versus a gastroenterologist?
If the primary complaint is frequent, severe head pain with clear neurological signs (visual aura, weakness), start with a neurologist. If gastrointestinal symptoms dominate and headaches appear after meals, a gastroenterologist can screen for intolerances and gut inflammation first.

Rashi Shetty
September 29, 2025 AT 13:07It is evident that the gut‑brain axis, while scientifically intriguing, is often misrepresented by lay articles that conflate correlation with causation. A rigorous analysis demands that we differentiate between anecdotal associations and controlled clinical evidence. Moreover, the propensity to recommend broad dietary overhauls without individualized assessment betrays a simplistic moralizing stance toward nutrition. Readers should be cautioned against uncritical acceptance of such sweeping prescriptions.
Queen Flipcharts
September 30, 2025 AT 11:21One could argue that the very notion of a “gut‑brain conversation” reflects the broader struggle of a nation to harmonize its internal discord. The United States, as the epitome of freedom, must not capitulate to vague health trends that undermine personal responsibility. Only through disciplined, patriotic adherence to evidence‑based practices can we safeguard both our constitution and our constitution of the body.
Jason Peart
October 1, 2025 AT 09:34Hey folks, let me tell you a story about my own migraine‑gut rollercoaster that feels like a drama series.
It started with a lazy brunch of eggs and coffee, and within an hour my stomach sounded like a fireworks display.
I blamed the coffee at first, but the real villain was a sneaky dairy product that decided to revolt in my intestines.
The next thing I knew, a pounding pressure hit the back of my head like a drumroll from an angry band.
I tried the usual over‑the‑counter meds, but they barely whispered against the thunderstorm brewing inside.
So I grabbed a notebook and started tracking every bite, every sip, every mood swing, just like a detective on a case.
Turns out, when I ate a slice of pizza with extra cheese, my gut would groan and my brain would follow suit an hour later.
When I switched to a low‑FODMAP plan, the chaos subsided, and the migraines started taking a vacation.
I also learned that staying hydrated is not just a cliché; my body literally screamed for water after each episode.
I added a probiotic yogurt to my diet, and gradually the gut‑brain chatter turned from shouting to polite conversation.
Stress, of course, played its part, because when I worked late nights, my vagus nerve seemed to send SOS signals straight to my temples.
I began a simple breathing routine-four breaths in, four breaths out-and noticed the headache intensity drop like a dimming light.
The biggest lesson? Your gut is not a passive organ; it’s an active participant that can summon pain if you ignore its warnings.
So if you’re battling the same thing, start logging, stay consistent, and give your body a chance to speak.
Trust me, the payoff is worth the effort, and soon you’ll find yourself living with fewer “brain‑explosions” and more calm days.
Hanna Sundqvist
October 2, 2025 AT 07:47They don't tell you that the pharmaceutical companies are silencing the real cure-proper gut health-because a healthy population would cut into their profits. It's no coincidence that the studies are all funded by the same big players who want you to pop pills instead of fixing your diet. The whole gut‑brain narrative is just a smokescreen.
Jim Butler
October 3, 2025 AT 06:01Dear community, let us embrace the transformative power of mindful hydration and balanced nutrition 🌟. By committing to a daily water intake of at least two liters, you empower both your digestive tract and cerebral vessels. Incorporate probiotic‑rich foods to nurture a thriving microbiome, and observe the symphony of reduced abdominal discomfort and lighter-headedness. Together we can cultivate resilience and thrive!
Ian McKay
October 4, 2025 AT 04:14It is imperative to adhere strictly to grammatical precision when composing health advice.
Deborah Messick
October 5, 2025 AT 02:27While many laud the gut‑brain axis as a panacea for migraine sufferers, a prudent skeptic must question the extrapolation of limited mechanistic studies to broad clinical recommendations. The insistence on universal dietary restrictions may inadvertently engender nutritional deficiencies. Thus, one should advocate for personalized assessment rather than blanket prescriptive measures.
Jolanda Julyan
October 6, 2025 AT 00:41It is absolutely vital that you understand the simple truth behind this whole gut‑brain thing. Your stomach is not some passive bag of food; it actively communicates with the brain, and when you ignore that, you pay the price with throbbing headaches. The science is clear-serotonin made in the gut can trigger the migraine circuitry if things go awry. Stop falling for fancy jargon and start drinking enough water every single day, because dehydration is a cheap and easy trigger that many overlook. Eat regular, balanced meals instead of bingeing on processed junk that inflames the gut lining. Incorporate a handful of probiotic foods like yogurt or kimchi to keep the microbes happy and the brain calm. Manage stress with short walks or breathing exercises; the vagus nerve will thank you and the migraines will lessen. Finally, if you continue to suffer despite these basic steps, seek professional guidance rather than endlessly scrolling forums.
Emily Rossiter
October 6, 2025 AT 22:54Your efforts to log symptoms and adjust lifestyle are commendable, and the consistency you maintain will likely reveal patterns that are otherwise hidden. Keep the diary up‑to‑date, and review it weekly to notice any correlations between meals, stressors, and headache intensity.
Renee van Baar
October 7, 2025 AT 21:07I appreciate the vivid account you shared; your systematic tracking truly embodies the inclusive mentorship we need.
Mithun Paul
October 8, 2025 AT 19:21The critique you present, while formally articulated, neglects the pragmatic realities faced by individuals dealing with overlapping gastrointestinal and neurological symptoms; a more nuanced analysis would consider patient heterogeneity.
Sandy Martin
October 9, 2025 AT 17:34While your concerns about industry influence are understandable, it is essential to base conclusions on peer‑reviewed evidence rather than conjecture, ensuring that recommendations remain scientifically sound.
Steve Smilie
October 10, 2025 AT 15:47Indeed, the epistemic rigor you champion elevates discourse beyond mere suspicion, inviting a kaleidoscopic exploration of gut‑brain interdependence that transcends reductionist paradigms.