How to Understand Biosimilars and Their Cost Implications

Biologic drugs can cost $7,000 a month. For conditions like rheumatoid arthritis, Crohn’s disease, or certain cancers, these treatments are life-changing-but also life-draining financially. That’s where biosimilars come in. They’re not generics. They’re not copies. They’re highly similar versions of complex biologic medicines, approved by the FDA to work just as safely and effectively. And they’re already cutting costs for millions of patients in the U.S.
What Exactly Are Biosimilars?
Biosimilars are made from living cells-yeast, bacteria, or animal cells-not chemicals. That’s why they’re not like the little white pills you pick up at the pharmacy. A generic version of aspirin is chemically identical to brand-name aspirin. But a biosimilar? It’s like saying two handmade leather jackets look and feel nearly the same, even if stitched by different artisans. The materials and process matter. The FDA defines a biosimilar as having no clinically meaningful differences from its reference biologic in safety, purity, and potency. That’s not marketing speak. It’s backed by years of testing: structural analysis, animal studies, human blood tests, and sometimes full clinical trials. The goal? Prove that switching won’t cause unexpected side effects or reduced effectiveness. The first U.S. biosimilar, Zarxio (a filgrastim product), got FDA approval on March 6, 2015. Since then, 45 biosimilars have been approved as of October 2023. They treat cancer, autoimmune diseases, diabetes, and more. And the science is solid. Studies like the NOR-SWITCH trial, published in The Lancet, found no increase in immune reactions or loss of effectiveness when patients switched from reference biologics to biosimilars.How Do Biosimilars Save Money?
Here’s the big one: biosimilars cost less. But not as much as you might think. Generic small-molecule drugs-like metformin or lisinopril-can cut prices by 80-85%. Biosimilars? They typically save 15-30% at launch. That might seem low, but when the original drug costs $7,000 a month, even a 20% discount means $1,400 saved per patient, every month. Take Humira. Before biosimilars hit the market in 2023, it was the most expensive drug in the U.S., with a list price of $7,000 per month. The first interchangeable biosimilar, Hyrimoz, launched at $5,054-a 28% drop. Other biosimilars followed, pushing prices down further. Express Scripts reported that in the first year, Humira biosimilars reduced average net prices by over 35%. And it’s not just list prices. The Inflation Reduction Act of 2022 cut Medicare Part D cost-sharing for biosimilars to just 25% starting in 2024. For seniors on fixed incomes, that’s huge. One patient with rheumatoid arthritis told the Arthritis Foundation: “My copay went from $1,200 to $300. I didn’t have to choose between my medicine and groceries anymore.” The RAND Corporation estimates biosimilars could save the U.S. healthcare system $54 billion between 2017 and 2026. By 2030, the Congressional Budget Office projects savings could hit $150 billion annually-if market barriers are cleared.Why Aren’t Biosimilars Cheaper Everywhere?
If they work and save money, why aren’t they everywhere? One reason: patents. Biologic makers use legal tactics-like “product hopping” or filing dozens of minor patents-to delay biosimilar entry. For example, while 72% of new infliximab (Remicade) prescriptions went to biosimilars within 18 months, only 28% did for etanercept (Enbrel), because of aggressive patent litigation. Another issue: payer rules. Insurance companies sometimes don’t automatically cover biosimilars unless you try the brand first. Or they make you jump through hoops-prior authorization, step therapy, paperwork. A 2022 ASCO survey found that 78% of oncologists spent 1-2 hours learning how to navigate these payer requirements. And then there’s the “interchangeable” label. Only six biosimilars had this status as of November 2023. An interchangeable biosimilar can be substituted at the pharmacy without the doctor’s approval-just like a generic. But most biosimilars still need a doctor to specifically prescribe them. Forty-eight states have laws governing substitution, but rules vary. In some places, pharmacists must notify the prescriber. In others, they can’t substitute at all without permission.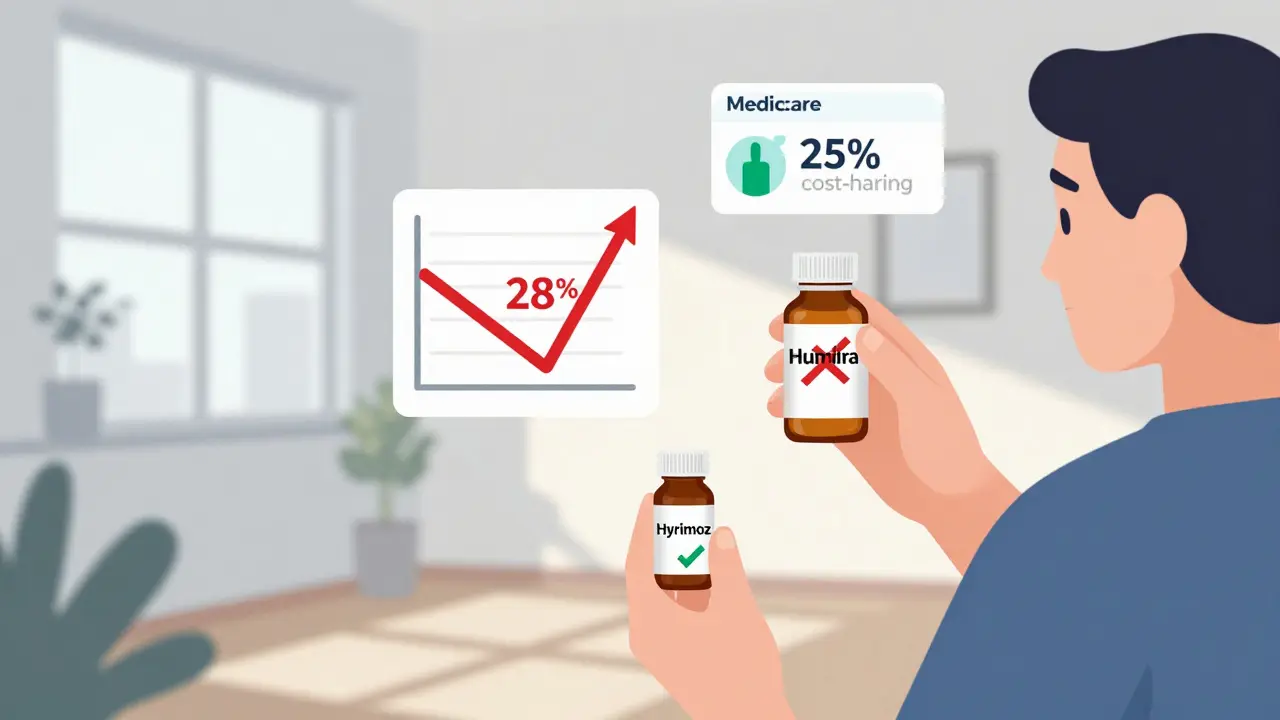
Are Biosimilars Safe? What Do Patients Say?
Fear is the biggest barrier to adoption-not science. A 2022 Arthritis Foundation survey of 1,200 patients found that 87% reported no difference in effectiveness compared to the original biologic. Seventy-two percent said their out-of-pocket costs dropped. But 28% were initially worried. That’s not about the science. It’s about trust. Reddit threads in r/rheumatology are full of questions: “Will my flare come back?” “Is this just a cheaper version?” Rheumatologists are answering. One top commenter, DrRheumMD, said: “I spend 10-15 minutes per patient explaining the evidence. The data is clear. But I get why they’re scared.” Patient reviews on Drugs.com for Renflexis (a biosimilar to Remicade) average 4.2 out of 5 stars. Common praises: “Same results, half the cost.” Common complaints: “Insurance won’t cover it.” Not efficacy. Coverage. The European Medicines Agency has tracked biosimilars for over 16 years. No new safety signals. No unexpected reactions. The FDA says the same: “Biosimilars are as safe and effective as their reference products.”What’s Next for Biosimilars?
The pipeline is full. Seven biosimilar applications are pending for Stelara (ustekinumab), a $10,000-a-month drug for psoriasis and Crohn’s. When they launch, savings could be massive. The global biosimilars market is projected to grow from $9.3 billion in 2022 to $33.3 billion by 2028. The U.S. is catching up, but still lags behind Europe. In Europe, biosimilars captured 84% of the filgrastim market within three years. In the U.S., it’s 65%. Why? Europe has simpler pricing, stronger government negotiation, and fewer patent barriers. The U.S. system is fragmented-pharmacies, insurers, PBMs, hospitals-all with different rules. Future biosimilars may even get better. “Biobetters”-next-gen biologics with improved dosing or longer-lasting effects-are already in development. These won’t be biosimilars. They’ll compete with both the original and the biosimilar.How to Use Biosimilars Wisely
If you’re on a biologic and your doctor mentions a biosimilar:- Ask: “Is there a biosimilar for my drug?”
- Ask: “Is it interchangeable?”
- Ask: “Will my insurance cover it?”
- Ask: “What’s the evidence for switching?”
Bottom Line
Biosimilars aren’t a magic fix. They won’t make all biologics cheap overnight. But they’re the most powerful tool we have right now to make life-saving treatments affordable. They’re safe. They’re effective. And they’re saving real people real money. The next time you hear someone say, “It’s just a copy,” remind them: it’s a copy that went through 12 years of research, 100+ lab tests, and thousands of patient studies to prove it works just as well. And it’s helping patients breathe easier, walk farther, and live longer-without going bankrupt.Are biosimilars the same as generic drugs?
No. Generics are chemically identical copies of small-molecule drugs, like aspirin or metformin. Biosimilars are made from living cells and cannot be exact copies. They’re highly similar to their reference biologic, with no clinically meaningful differences in safety or effectiveness, but they’re more complex to produce and test.
Do biosimilars cause more side effects than the original biologic?
No. Major studies, including the NOR-SWITCH trial and long-term data from the European Medicines Agency, show no increased risk of side effects or immune reactions when switching to a biosimilar. The FDA requires extensive testing to ensure safety before approval.
Why aren’t biosimilars cheaper in the U.S. than in Europe?
The U.S. has more patent litigation, complex payer rules, and less government price negotiation. In Europe, governments set prices and encourage competition. In the U.S., insurers, PBMs, and manufacturers negotiate behind closed doors, which slows price drops. European markets saw 84% adoption of filgrastim biosimilars in three years; the U.S. reached 65%.
Can my pharmacist switch my biologic to a biosimilar without my doctor’s approval?
Only if the biosimilar is labeled as “interchangeable” and your state allows substitution. As of 2023, only six biosimilars had interchangeable status in the U.S. Even then, 48 states have laws requiring notification, consent, or documentation. In most cases, your doctor must specifically prescribe the biosimilar.
How do I know if a biosimilar is right for me?
Talk to your doctor. Ask if a biosimilar exists for your current biologic, whether it’s interchangeable, and how your insurance covers it. Check the FDA’s Purple Book for approved products. Most patients report no difference in effectiveness, and many see lower out-of-pocket costs. But your medical history matters-your provider can help weigh the risks and benefits.
Will switching to a biosimilar affect my treatment results?
For most patients, no. Clinical trials and real-world data show biosimilars work just as well as the original biologic. Studies involving thousands of patients with cancer, arthritis, and inflammatory bowel disease found no loss of effectiveness. A small number may feel anxious after switching, but that’s usually psychological-not biological.
What’s the difference between a biosimilar and a biobetter?
A biosimilar is designed to be highly similar to an existing biologic. A biobetter is a new, improved version of a biologic-maybe with longer-lasting effects, fewer side effects, or easier delivery. Biobetters aren’t biosimilars; they’re next-generation drugs that compete with both the original and the biosimilar.

Jodi Harding
January 16, 2026 AT 15:21This isn't just about money-it's about dignity. I watched my mom choose between her Humira and groceries for three years. When the biosimilar hit, she cried. Not from sadness-from relief. No one should have to beg for the right to live.
Tyler Myers
January 16, 2026 AT 15:42Let’s be real-biosimilars are Big Pharma’s Trojan horse. They’ve been pushing this ‘same efficacy’ nonsense for decades while the real drug prices keep climbing. The FDA’s approval process? A rubber stamp for lobbyists. You think they’d let a ‘copy’ through if it didn’t help them control the market? Wake up. This is corporate engineering disguised as progress.
Nishant Sonuley
January 17, 2026 AT 14:15Y’all in the US are acting like this is some new miracle. In India, we’ve had biosimilars for over a decade-infliximab, rituximab, even trastuzumab for breast cancer-all at 1/10th the price. I remember my uncle getting his biologic in Mumbai for $200/month. Here? Same drug, $5,000. The difference isn’t science-it’s greed wrapped in insurance paperwork. And don’t get me started on how PBMs milk every penny. We need to stop treating healthcare like a stock market and start treating it like a human right. Also, side note: the NOR-SWITCH trial? Brilliant. Should be mandatory reading for every med student.
Andrew McLarren
January 19, 2026 AT 03:49While the economic and clinical arguments in favor of biosimilars are compelling, it is imperative to acknowledge the structural and regulatory impediments that continue to hinder equitable access. The fragmentation of payer systems, inconsistent state-level substitution laws, and the persistence of patent evergreening collectively undermine the potential societal benefits of these therapeutics. A unified, evidence-based national policy framework-anchored in transparency and patient-centered outcomes-is not merely advisable; it is ethically obligatory.
Andrew Short
January 20, 2026 AT 20:51Stop pretending this isn’t a scam. Biosimilars are just the next phase of pharma’s playbook: make the original drug outrageously expensive, then release a ‘similar’ version at a slightly lower price to look like they’re being nice. Meanwhile, they’re still charging you $1,200 copays because your insurance doesn’t want to deal with the paperwork. And don’t even get me started on how they use ‘interchangeable’ as a buzzword to trick patients into thinking it’s safe when half the states won’t even let pharmacists switch it without a doctor’s signature. It’s not innovation-it’s exploitation with a lab coat.
christian Espinola
January 21, 2026 AT 02:57Correction: The FDA does NOT approve biosimilars as ‘equivalent’-they approve them as ‘highly similar.’ The distinction matters. You’re not getting the same molecule. You’re getting a molecule that behaves similarly under controlled conditions. Real-world variability? Not tracked long-term. And those ‘no difference’ studies? Mostly 6-month trials. What about autoimmune flares that emerge after 18 months? No one’s looking. Also, ‘interchangeable’ is a marketing term, not a clinical guarantee. And your ‘4.2-star’ Drugs.com rating? Half those reviews are from people who never even tried the original. Anecdotes aren’t data. And data? Still incomplete.
Chuck Dickson
January 22, 2026 AT 15:49Hey, if you’re on a biologic and your doc says there’s a biosimilar? DO IT. Seriously. I switched from Enbrel to a biosimilar last year. No flare-ups. No weird side effects. My copay dropped from $900 to $210. I’m not a scientist-I’m just a guy who didn’t want to go broke. And guess what? I’m still alive. Still hiking. Still playing with my kids. Biosimilars aren’t magic, but they’re the closest thing we’ve got to justice in this broken system. If your doctor says it’s safe, trust them. And if your insurance fights you? Fight back harder.
Dayanara Villafuerte
January 24, 2026 AT 04:38OMG I just switched to a biosimilar and my insurance actually covered it 😭 I thought I’d have to sell a kidney. Now I can afford to eat veggies again 🥦💖 #BiosimilarsSaveLives #NotJustACopy