How Echocardiography Detects Left Ventricular Dysfunction
Echocardiography is a non‑invasive cardiac imaging technique that uses ultrasound waves to create real‑time pictures of the heart. By visualizing chamber size, wall motion, and blood flow, it helps clinicians spot left ventricular dysfunction early enough to start treatment.
Why Left Ventricular Function Matters
The left ventricle (LV) is the heart’s main pump. When its ability to contract drops, blood backs up into the lungs, causing breathlessness and fatigue. Left Ventricular Dysfunction (LVD) covers a spectrum from mild systolic impairment to severe heart failure.
Core Echo Measurements for LV Assessment
Two numbers dominate echo reports:
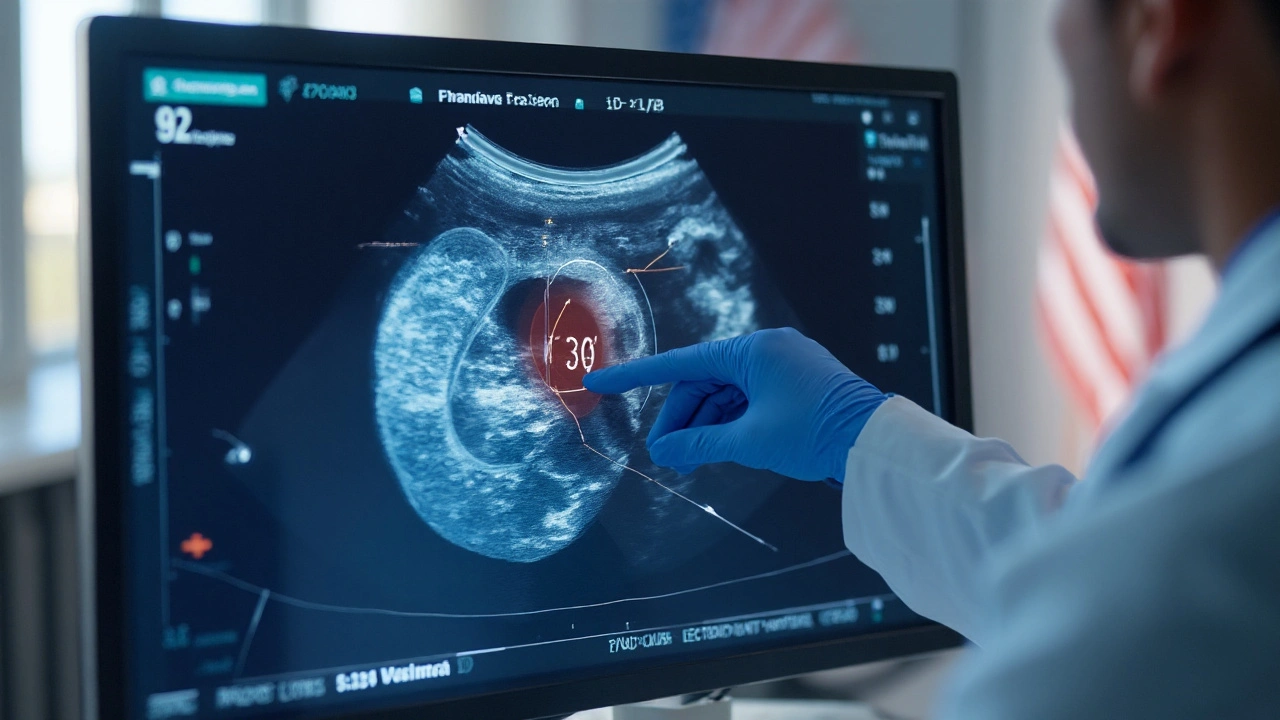
- Left Ventricular Ejection Fraction (LVEF) measures the percentage of blood expelled with each beat. Normal is 55‑70%; values below 40% signal systolic dysfunction.
- Global Longitudinal Strain (GLS) tracks myocardial fiber shortening. A GLS of -18% or better is typical; less negative values indicate subtle contractile loss that LVEF may miss.
Both figures come from 2D Echocardiography, the most common echo view. The modality captures cross‑sectional slices of the heart and feeds them into automated software that traces end‑diastolic and end‑systolic borders (Simpson’s biplane method).
Advanced Echo Techniques
When standard 2D images are borderline, clinicians turn to newer tools:
- Doppler Echocardiography evaluates blood velocity, helping quantify regurgitation or stenosis that can burden the LV.
- Speckle Tracking Echocardiography follows natural acoustic markers (speckles) across frames, delivering strain measurements in multiple directions (longitudinal, circumferential, radial).
- Transesophageal Echocardiography (TEE) inserts a probe into the esophagus for clearer images of posterior structures, useful when chest wall interference limits transthoracic views.
How Echo Stacks Up Against Other Cardiac Tests
| Modality | Spatial Resolution | Temporal Resolution | Availability | Key Strength |
|---|---|---|---|---|
| 2D Echo | Moderate | High (50‑90fps) | Widely available | Real‑time function, bedside |
| TEE | High | High | Specialized | Better posterior view |
| Speckle Tracking | Moderate | High | Requires software | Detects subclinical dysfunction |
| Cardiac MRI | Very high | Low (20‑30fps) | Limited sites | Gold‑standard volumes, tissue characterization |
Echo wins on speed and cost, but MRI remains the reference for precise volumetrics and scar detection. When echo results are ambiguous, many guidelines (ACC/AHA) suggest confirming with cardiac MRI or measuring biomarkers like B‑type Natriuretic Peptide (BNP), which rises with ventricular pressure overload.
Real‑World Scenarios
Case 1 - Silent systolic impairment: A 58‑year‑old smoker comes for a routine check. LVEF on 2D echo reads 52%, just under the lower limit of normal. GLS measures -14%, revealing early contractile loss. The clinician starts low‑dose ACE‑inhibitor therapy, preventing progression.
Case 2 - Diastolic heart failure: A 72‑year‑old woman reports breathlessness with preserved LVEF (65%). Doppler inflow patterns show an E/A ratio >2 and elevated left atrial pressure, confirming diastolic dysfunction. Management focuses on blood pressure control and lifestyle changes.
Case 3 - Post‑MI remodeling: A 45‑year‑old man suffers a myocardial infarction. Serial echoes track LV end‑diastolic volume increase from 120ml to 150ml over three months, flagging adverse remodeling. Intensified beta‑blocker therapy and cardiac rehab are initiated.
Limitations of Echo and When to Add Other Tests
Even the best operator can run into obstacles:
- Obesity or chronic lung disease may degrade acoustic windows, reducing image quality.
- Rapid arrhythmias (e.g., atrial fibrillation) make beat‑to‑beat averaging necessary, which can blur small changes.
- Scar tissue assessment is limited; cardiac MRI or nuclear perfusion studies provide tissue characterization.
In such cases, combine echo with Cardiac MRI for volumetric precision, or check serum BNP to corroborate functional findings.
Quick Checklist for Interpreting Echo in LV Dysfunction
- Confirm image quality: clear endocardial borders in apical 4‑chamber and 2‑chamber views.
- Calculate LVEF using Simpson’s biplane method; note any discrepancy with visual estimate.
- Measure GLS if software is available; compare with age‑adjusted normal (≈ -18%).
- Assess Doppler inflow (E/A ratio) and tissue Doppler (eʹ) for diastolic function.
- Look for regional wall motion abnormalities that may point to prior infarction.
- Document LV size (end‑diastolic dimension) and wall thickness for hypertrophy evaluation.
- If image quality is poor, recommend TEE or cardiac MRI as follow‑up.
Connecting the Dots: Related Topics to Explore
Understanding echo opens doors to several adjacent areas:
- Heart Failure Management - pharmacologic and device therapies guided by echo data.
- Cardiomyopathy Classification - differentiating ischemic vs. dilated vs. hypertrophic forms.
- Guideline‑Directed Medical Therapy - ACC/AHA recommendations that hinge on LVEF thresholds.
- Advanced Strain Imaging - research on predictive value for chemotherapy‑induced cardiotoxicity.
Each of these topics deepens the clinician’s ability to translate echo findings into concrete patient‑centered actions.

Frequently Asked Questions
What is the normal range for left ventricular ejection fraction?
A healthy adult typically has an LVEF between 55% and 70%. Values below 50% suggest systolic dysfunction, while values above 70% may indicate hyperdynamic circulation.
Can echocardiography detect early heart failure before symptoms appear?
Yes. Techniques like speckle‑tracking strain can uncover subtle myocardial impairment even when LVEF is still normal. Early detection allows timely lifestyle and pharmacologic interventions.
When should I order a cardiac MRI instead of an echo?
Consider MRI when echo windows are poor, when precise volumetry is critical (e.g., pre‑surgical planning), or when tissue characterization (scar, fibrosis) is needed. MRI also serves as a reference when echo measurements are inconsistent.
How reliable is GLS compared to LVEF?
GLS is more sensitive for detecting subclinical dysfunction. Studies show that a reduction of >2% in GLS predicts adverse outcomes even when LVEF remains above 50%.
Does obesity affect the accuracy of echocardiographic measurements?
Yes. Excess adipose tissue can attenuate ultrasound beams, leading to suboptimal endocardial delineation. In such cases, contrast agents or alternative imaging (TEE, MRI) improve accuracy.

Alex Jhonson
September 25, 2025 AT 06:32Great summary, especially the part on strain imaging.
Macy Weaver
October 2, 2025 AT 16:52The breakdown of LVEF versus GLS really helps me see why strain is gaining traction. I appreciate the clear checklist that walks you through image quality before diving into numbers. It’s also handy to have the diastolic section tucked in there for those with preserved EF. Overall, a solid primer for anyone brushing up on echo basics.
James McCracken
October 10, 2025 AT 03:12One might argue that the obsession with numerical thresholds reduces the heart to a mere calculator output. Yet the article dutifully lists percentages as if they were moral absolutes. While the tables are tidy, they mask the underlying variability inherent in any ultrasound acquisition. A more nuanced discussion about operator dependence would have elevated the piece beyond a checklist. As it stands, it feels like a bureaucratic script rather than an exploration of cardiac physiology.
Evelyn XCII
October 17, 2025 AT 13:32Oh sure, because we all have infinite time to chase GLS numbers while the patient waits in the hallway.
Suzanne Podany
October 24, 2025 AT 23:52Love how the article emphasizes real‑time bedside utility - that’s where echo truly shines. The step‑by‑step guide for image acquisition is spot‑on for trainees. Remember to always double‑check endocardial borders; a missed slice can skew the Simpson calculation. Adding a quick tip about contrast agents for poor windows would be icing on the cake. Kudos to the author for making a dense topic approachable.
Nina Vera
November 1, 2025 AT 09:12This piece reads like a backstage pass to the echo lab, and I’m here for every curtain raise! From the flashy speckle‑tracking graphics to the quiet heroics of Doppler flow, each technique gets its moment in the spotlight. The case studies feel like mini‑dramas, especially the silent systolic impairment that sneaks past a borderline EF. I could almost hear the echo machine humming as the LV volume swells in the post‑MI remodeling saga. The comparison table is the perfect plot twist, showing where MRI steals the show. Keep the hype alive, because better echo awareness means earlier interventions. Seriously, if this weren’t a medical article, I’d binge‑read it for the narrative alone.
Ellie Haynal
November 8, 2025 AT 19:32The moral of the story is clear: ignoring subtle strain changes is a disservice to patients. When we rely solely on LVEF, we risk missing the early warning signs that could change a life trajectory. The article does well to highlight that, but it could have pushed harder for routine GLS adoption in community practices. Still, the emphasis on combining modalities when windows are poor reflects a responsible approach. Let’s champion this proactive mindset across all cardiology units.
Jimmy Gammell
November 16, 2025 AT 05:52Hey team, great job breaking down the echo toolbox! 👍 When you hit a tough acoustic window, remember to try a low‑frequency probe or consider a contrast agent to boost endocardial definition. Keep practising the Simpson biplane method – muscle memory wins the day. And don’t forget to have a little fun with the speckle tracking – it’s like watching tiny fireworks inside the heart! 🌟
fred warner
November 23, 2025 AT 16:12The article succinctly captures why echo remains the workhorse of cardiac imaging. Its high temporal resolution allows us to witness the heart’s dynamics beat by beat. By juxtaposing echo against MRI, the author clarifies where each modality excels. The inclusion of BNP as a complementary biomarker rounds out a comprehensive diagnostic pathway. Readers should feel empowered to integrate these tools into everyday practice.
Carlise Pretorius
December 1, 2025 AT 02:32nice rundown of echo vs mri its clear echo wins on speed and cost but mri still gold for scar detection love the case examples especially the post mi remodeling keep it up
Johnson Elijah
December 8, 2025 AT 12:52🚀 This guide nails the essentials for spotting left ventricular dysfunction early. 🎯 Highlighting GLS as a subclinical marker is especially useful for high‑risk patients. The checklist format makes it easy to embed into daily rounds. When echo windows are poor, the recommendation to jump to TEE or MRI is spot‑on. Let’s keep pushing for broader GLS adoption across all echo labs! 💪
Roxanne Lemire
December 15, 2025 AT 23:12The distinction between systolic and diastolic dysfunction presented here mirrors the age‑old philosophical dichotomy of form versus function. While numbers like LVEF provide a quantifiable form, strain offers insight into the underlying functional integrity. Both are necessary to grasp the heart’s true state. The article’s balanced tone respects this duality without privileging one over the other.
Alex Mitchell
December 23, 2025 AT 09:32Appreciate the thorough walk‑through of each echo modality. The stepwise checklist will help novice sonographers avoid common pitfalls. Remember to document image quality scores; they’re handy when you need to justify a repeat study. If you encounter suboptimal windows, a quick TEE or contrast echo can save a lot of time. Good job keeping the information both practical and precise. 🙂
Narayan Iyer
December 30, 2025 AT 19:52From a hemodynamic standpoint, the article does a bang‑up job of correlating Doppler velocity profiles with left atrial pressure estimates. The GLS metric, expressed in negative percent, serves as a sensitive biomarker for myocardial contractile reserve. For institutions lacking speckle‑tracking software, the author wisely suggests leveraging tissue Doppler e′ as a surrogate. Overall, the piece is a solid compendium for both the seasoned cardiologist and the budding echo technologist.
Amanda Jennings
January 7, 2026 AT 06:12Really liked how the piece kept things laid‑back yet informative. The cases felt relatable, especially the silent systolic impairment scenario. It’s good to see a reminder that even a marginal dip in EF can have big clinical implications. Looking forward to more posts that blend tech details with real‑world applications.
alex cristobal roque
January 14, 2026 AT 16:32Let me walk you through why echocardiography remains the cornerstone of left ventricular assessment, starting with the physics of ultrasound and how it translates into real‑time imaging of myocardial motion. First, the transducer emits high‑frequency sound waves that penetrate the thoracic wall and reflect off tissue interfaces, creating echoes that are reconstructed into grayscale images; this fundamental principle underlies every 2‑D view we acquire at the bedside. Second, when we apply the Simpson’s biplane method, we trace the endocardial border in both apical four‑ and two‑chamber views, which the machine then integrates to calculate end‑diastolic and end‑systolic volumes, ultimately yielding the ejection fraction. Third, strain imaging-particularly global longitudinal strain-leverages speckle‑tracking algorithms that follow natural acoustic markers across the cardiac cycle, providing a quantitative measure of myocardial fiber shortening that can detect dysfunction before EF falls below the conventional 50 % threshold. Fourth, Doppler techniques add a hemodynamic dimension by measuring blood flow velocities, allowing us to assess valvular regurgitation, stenosis, and even diastolic filling patterns through parameters such as E/A ratio and tissue Doppler e′ velocity. Fifth, when acoustic windows are compromised by obesity, lung disease, or body habitus, contrast agents can be injected to enhance endocardial border delineation, dramatically improving measurement accuracy. Sixth, for patients with suboptimal transthoracic windows, transesophageal echocardiography offers superior resolution of posterior structures, albeit at the cost of invasiveness and need for sedation. Seventh, the integration of three‑dimensional echo is expanding, giving us volumetric datasets that reduce geometric assumptions inherent in 2‑D calculations, though widespread adoption is limited by equipment cost and learning curve. Eighth, it’s crucial to remember that all these measurements are operator dependent; adherence to standardized acquisition protocols and regular quality assurance audits are essential to maintain reproducibility. Ninth, while cardiac MRI is hailed as the gold standard for volumetrics and tissue characterization, its limited availability, higher expense, and longer scan times make echo the pragmatic first‑line choice in most clinical settings. Tenth, the clinical impact of early detection cannot be overstated-identifying subtle strain abnormalities can prompt initiation of guideline‑directed medical therapy, potentially altering disease trajectory. Eleventh, ongoing research is exploring how artificial intelligence can automate border detection and strain analysis, promising to reduce inter‑observer variability and streamline workflow. Twelfth, the article’s checklist is an excellent tool, but I would add a reminder to record the frame rate of the acquisition, as low temporal resolution can blur rapid wall motion and underestimate strain. Thirteenth, documentation of image quality scores alongside numerical results provides context for future comparisons, especially in longitudinal follow‑up. Fourteenth, education and hands‑on training remain the bedrock of high‑quality echo labs; simulation platforms and mentorship programs can accelerate skill acquisition. Finally, keep in mind that echocardiography is not just a diagnostic test but a dynamic decision‑making engine that informs treatment, risk stratification, and patient counseling throughout the continuum of cardiovascular care.
Bridget Dunning
January 22, 2026 AT 02:52The composition adeptly synthesizes contemporary echo methodology with established guideline thresholds, offering a comprehensive resource for clinicians. Its meticulous delineation of LVEF and GLS metrics, coupled with an evidence‑based discussion of Doppler indices, underscores the article’s scholarly rigor. The inclusion of case vignettes provides pragmatic context, facilitating translation of theoretical concepts into bedside practice. I commend the author for maintaining a balance between technical depth and accessibility, thereby catering to both seasoned cardiologists and trainees.
Shweta Dandekar
January 29, 2026 AT 13:12While the exhaustive enumeration of echo techniques is commendable, one must not lose sight of the ethical imperative to prioritize patient comfort over technological flamboyance; the over‑reliance on contrast agents and invasive TEE, as highlighted, should be judiciously calibrated to each clinical scenario, lest we inadvertently subject patients to unnecessary risk.