Diabetes and Thyroid Disease: Overlapping Symptoms and How to Manage Both
When your body’s energy system starts acting up, it’s easy to blame one thing - maybe you’re just tired, or your blood sugar is out of whack. But what if it’s not just one problem? What if your diabetes and your thyroid are both whispering the same warning signs at the same time? That’s more common than you think. About 30% of people with diabetes also have a thyroid disorder, and nearly 15% of those with thyroid issues also have diabetes. These aren’t random coincidences. They’re linked by biology, immune system mistakes, and shared symptoms that can trick even experienced doctors.
Why Diabetes and Thyroid Disease Keep Showing Up Together
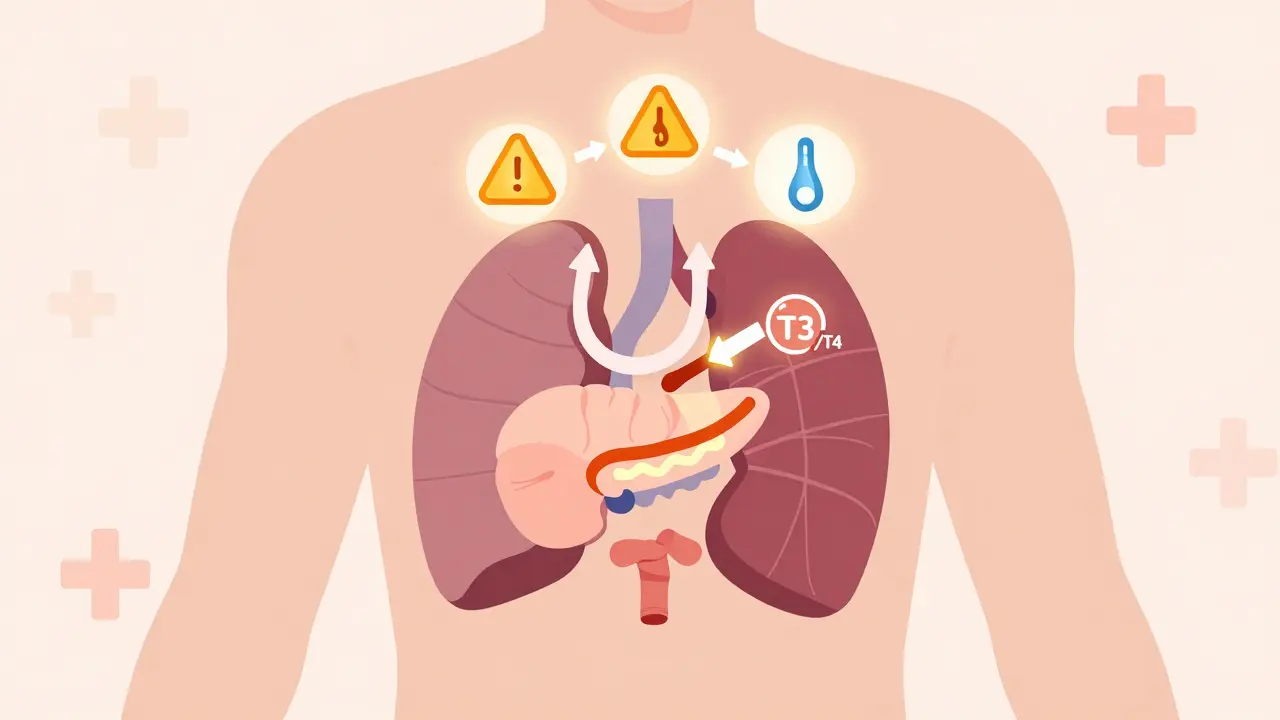
Your thyroid controls your metabolism - how fast your body burns fuel. Your pancreas controls insulin - how your body stores or uses that fuel. When one goes off, the other usually follows. In Type 1 diabetes, your immune system attacks the insulin-producing cells. In Hashimoto’s or Graves’ disease, it attacks your thyroid. Same faulty switch, different target. That’s why people with Type 1 diabetes are 5 to 10 times more likely to develop thyroid disease than someone without diabetes. Even Type 2 diabetes isn’t safe. Studies show people with Type 2 have a 21.9% chance of having thyroid dysfunction, compared to just 16.96% in the general population. Why? Because chronic high blood sugar causes inflammation, which can trigger or worsen autoimmune thyroid conditions. On the flip side, an underactive thyroid slows down how your body uses glucose, making insulin resistance worse. An overactive thyroid speeds up glucose use, causing unpredictable drops in blood sugar - even if you’re eating normally.The Symptoms You Can’t Ignore
Both conditions can make you feel like you’re falling apart - but in similar ways. Here’s what they share:- Unexplained weight changes: Losing weight without trying? Could be hyperthyroidism. Gaining weight despite eating less? Could be hypothyroidism. In people with both conditions, this happens in 65-70% of cases.
- Fatigue: Not just ‘I stayed up late’ tired. This is bone-deep exhaustion that doesn’t go away with sleep. Reported in 78% of people managing both diseases.
- Hair loss: Thinning hair or patches? Not just stress. Thyroid hormones directly affect hair follicles. Seen in 42% of coexisting cases.
- Mood swings and depression: Feeling down, irritable, or numb? Thyroid imbalance affects serotonin and dopamine. Depression occurs in 29% of these patients.
- Temperature sensitivity: Always cold? Hypothyroidism. Sweating through your shirt in a cool room? Hyperthyroidism. 61% of people with both report this.
The Hidden Danger: Hypothyroidism Hiding Hypoglycemia
One of the most dangerous overlaps? Hypothyroidism can mask low blood sugar. Normally, when your blood sugar drops, your body releases adrenaline - you feel shaky, sweaty, your heart races. But if your thyroid is underactive, that adrenaline response is dampened. You might feel dizzy or confused - and think it’s just ‘being tired.’ Data from Tampa Bay Endocrine Institute shows 41% of diabetic patients with undiagnosed hypothyroidism had at least one severe hypoglycemic episode they didn’t recognize until it was too late. One patient, SugarFree87 on DiabetesDaily.com, described it perfectly: “After my hypothyroidism diagnosis, my insulin needs dropped by 30% overnight. I had three low blood sugar episodes in a week. No warning signs. Just blacking out.” Hyperthyroidism creates the opposite problem: your body burns through glucose too fast. Insulin gets cleared from your system 20-25% faster. That means you might need up to 30% more insulin than usual - or you’ll keep crashing. If your doctor doesn’t know your thyroid status, they’ll keep increasing your insulin dose, thinking you’re becoming more insulin resistant - when really, your thyroid is speeding everything up.
What Doctors Miss - And What You Should Ask For
A 2022 survey by the American Association of Clinical Endocrinologists found that 68% of endocrinologists admit they struggle to tell whether symptoms come from diabetes complications or thyroid problems. That’s why so many patients get misdiagnosed. One Reddit user from r/Thyroid shared: “I was told my blurred vision and numb hands were diabetic neuropathy. Turns out, my TSH was 12.5 - way above normal. My thyroid was the real culprit.” Here’s what you need to ask for - and when:- At diagnosis: Request a TSH test and thyroid antibody tests (TPOAb and TgAb). The American Diabetes Association now recommends this for all Type 1 diabetics and high-risk Type 2 patients.
- If you’re already diagnosed: Get your TSH checked every 6 months if you have diabetes, especially if your blood sugar is hard to control. Annual tests aren’t enough.
- If you’re on levothyroxine: Tell your doctor if you have gastroparesis (common in long-term diabetes). The drug absorbs 15-20% less if your stomach moves slowly.
Managing Both - Without Overloading Your Life
You don’t need to take ten pills and check your blood sugar 10 times a day. Smart management is about alignment. Medication adjustments: If your thyroid is underactive, your insulin needs often drop by 15-25%. If it’s overactive, they might rise by 20-40%. Always recheck your insulin dose after starting or changing thyroid meds. Diet matters more than you think: A 6-month trial published in PMC8787293 showed that following a Mediterranean diet - full of olive oil, fish, nuts, vegetables - improved HbA1c by 0.8-1.2% and lowered TSH by 0.5-0.7 mIU/L. That’s two conditions improving at once. Technology helps: Continuous glucose monitors (CGMs) are a game-changer. A 2022 JAMA study found people with both conditions using CGMs had 32% fewer hypoglycemic events and spent 27% more time in their target blood sugar range. Why? Because CGMs catch drops you don’t feel - especially when thyroid symptoms hide them.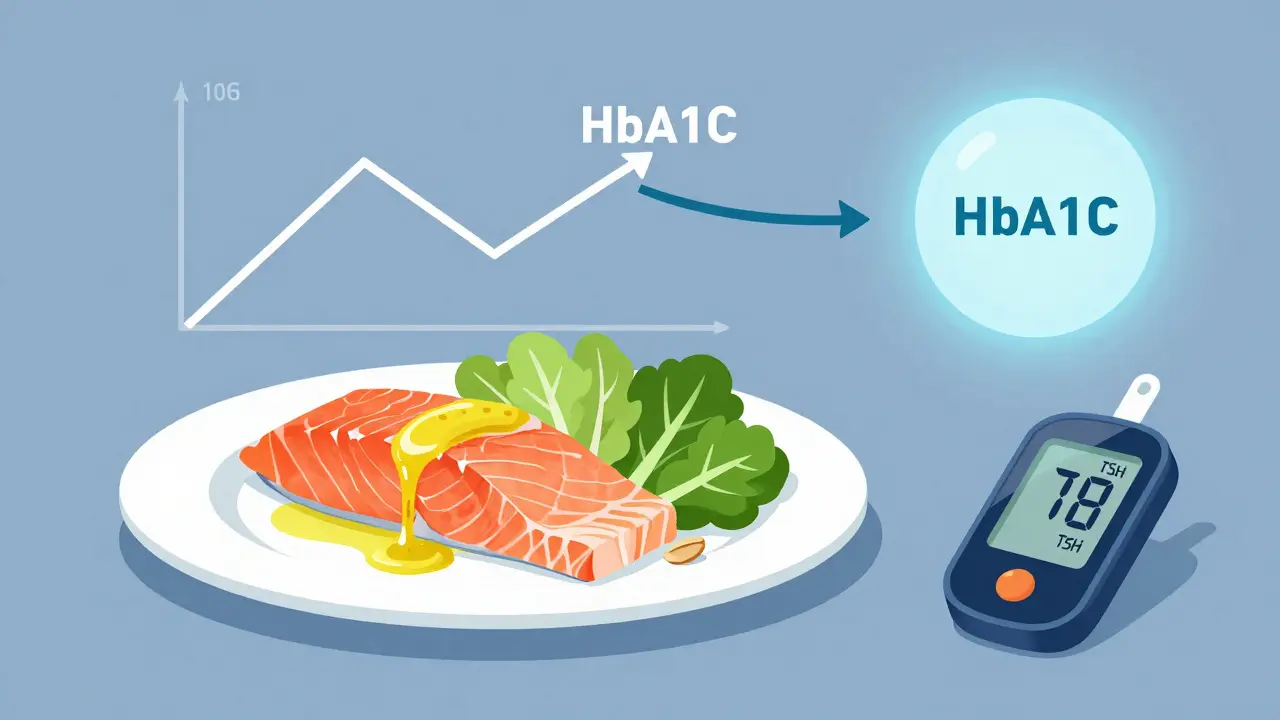
The Bigger Picture: Cost, Risk, and Hope
Having both conditions isn’t just inconvenient - it’s expensive. Patients pay $4,872 more per year in healthcare costs than those with diabetes alone. Why? More hospital visits, more eye exams, more heart tests. Thyroid dysfunction in diabetics increases the risk of retinopathy by 37.2% and raises LDL cholesterol by 18-22 mg/dL. But here’s the good news: treating the thyroid can cut hospital visits by 22% and ER trips by 17%, according to Harvard Medical School. A 2024 pilot study in Nature Communications found that GLP-1 receptor agonists - drugs like Ozempic - actually improved thyroid function in 63% of patients with subclinical hypothyroidism. New research is underway. The NIH’s TRIAD study, launched in early 2023, is tracking 5,000 people to see if early thyroid treatment can stop diabetes from getting worse. The American Association of Clinical Endocrinologists will release updated guidelines in October 2024 with clear algorithms for managing both conditions together.What to Do Today
If you have diabetes:- Ask your doctor for a TSH and thyroid antibody test - if you haven’t had one in the last year.
- Keep a symptom journal: note fatigue, weight changes, mood, temperature sensitivity.
- Don’t ignore unexplained blood sugar swings. They might be thyroid-related.
- If you’re on levothyroxine, take it on an empty stomach, 30-60 minutes before food - especially if you have gastroparesis.
- Consider a CGM if you’re struggling with lows or highs without clear patterns.
- Ask for a fasting glucose test and HbA1c - even if you feel fine.
- Monitor for increased thirst, frequent urination, or blurred vision.
- Let your endocrinologist know if you’re on insulin or metformin - dosing may need adjustment.
Can thyroid problems cause high blood sugar?
Yes. Hypothyroidism slows down how your body uses glucose, leading to insulin resistance and higher blood sugar levels. Studies show it can increase fasting glucose by 10-15% in people with Type 2 diabetes. Even mild thyroid underactivity can make diabetes harder to control.
Can diabetes cause thyroid problems?
Yes, especially Type 1 diabetes. Both are autoimmune diseases, so if your immune system attacks your pancreas, it’s more likely to attack your thyroid too. Type 2 diabetes increases inflammation, which can trigger thyroid dysfunction over time. About 1 in 3 people with diabetes will develop thyroid issues.
Should I get tested for thyroid disease if I have diabetes?
Absolutely. The American Diabetes Association recommends annual TSH testing for all Type 1 diabetics and high-risk Type 2 patients. If you’ve had diabetes for more than 5 years, or if your blood sugar is hard to control, ask for thyroid antibody tests too. Early detection prevents complications.
Can levothyroxine affect my blood sugar?
Yes. Starting levothyroxine can lower your insulin needs - sometimes dramatically. If you’re on insulin or other diabetes meds, your doctor should check your blood sugar closely in the first few weeks after starting or adjusting thyroid medication. A 30% drop in insulin needs isn’t rare.
What’s the best diet for someone with both diabetes and thyroid disease?
A Mediterranean-style diet works best. Focus on olive oil, fatty fish, nuts, vegetables, and whole grains. Avoid processed foods and excess sugar. Studies show this diet improves HbA1c by 0.8-1.2% and lowers TSH by 0.5-0.7 mIU/L in 6 months. It reduces inflammation - which helps both conditions.
Why do I feel worse when I start thyroid medication?
It’s often because your body is adjusting. If you have diabetes, starting levothyroxine can cause your insulin needs to drop suddenly. If you don’t reduce your insulin, you risk low blood sugar. Talk to your doctor before starting - they may need to adjust your diabetes meds at the same time.

Darryl Perry
January 13, 2026 AT 08:02This article is overly verbose. You don’t need 2000 words to say check your TSH if you’re diabetic. Simple. Done.
Windie Wilson
January 15, 2026 AT 00:59Oh wow, so my ‘diabetic fatigue’ was just my thyroid screaming into a pillow? Thanks for the 15-page novel, I guess. Now I can add ‘thyroid drama’ to my already full plate of medical nonsense.
Daniel Pate
January 16, 2026 AT 23:08The biological overlap here is fascinating. Autoimmune cross-reactivity isn’t just coincidence-it’s systemic failure of immune tolerance. The fact that insulin-producing beta cells and thyrocytes share antigenic triggers suggests a deeper immunological vulnerability than we’ve acknowledged. Why do we treat these as separate conditions when the root mechanism is identical? The medical model is still siloed, even as the biology screams unity.
Eileen Reilly
January 17, 2026 AT 07:19so like... if ur thyroid is chillin' and ur sugar is wild, maybe ur insulin is just confused? like why u keep doin' that?? i got a cgm now and it's like a drama queen but at least it tells me the truth. also levothyroxine made me pass out once bc i didnt change my insulin. oops. lol. #thyroidanddiabetes #sendhelp
Monica Puglia
January 18, 2026 AT 10:53Thank you for writing this. 🙏 I was diagnosed with Hashimoto’s last year and didn’t realize my blood sugar swings weren’t just ‘bad diabetes.’ My endo never mentioned thyroid testing. I’m so glad I found this. If you’re reading this and have diabetes-ask for the TSH. Seriously. It could save you from a lot of confusion and scary lows. You’re not alone. 💛
Cecelia Alta
January 18, 2026 AT 14:59Look, I’ve been managing both for 12 years and I can tell you this article is basically just a fancy brochure for endocrinologists trying to sell more tests. Yes, the stats are real. But here’s the truth: 90% of the time, your doctor doesn’t care unless you’re crashing. I’ve had three doctors tell me ‘it’s just stress’ or ‘you’re just not trying hard enough.’ You want to manage both? Stop listening to medical jargon and start tracking your symptoms like your life depends on it-which it does. Keep a journal. Note every time you feel off. Don’t wait for a lab report. Your body is screaming. Learn its language. And if your doctor rolls their eyes? Find a new one. No one else is going to fight for you. This isn’t about tests. It’s about survival. And if you’re not willing to be your own advocate? Then you’re already losing.
steve ker
January 18, 2026 AT 18:14Diabetes and thyroid same thing. People overthink. Check TSH. Take meds. Done. Why you write so much? Waste time.
Faith Wright
January 18, 2026 AT 21:54Steve Ker just said ‘done’ and walked away like he solved world hunger. Meanwhile, I spent 3 years getting misdiagnosed because no one connected my fatigue to my thyroid. So yeah. Maybe don’t reduce complex human biology to a single sentence. Just saying.