Carbohydrate Counting for Diabetes: A Complete Beginner’s Guide

Managing diabetes isn’t about cutting out carbs entirely-it’s about knowing how much and when you’re eating them. Carbohydrate counting, or carb counting, is one of the most effective, flexible, and widely recommended tools for people with diabetes who want to take control of their blood sugar. Whether you’re on insulin, taking oral meds, or just trying to stabilize your glucose levels, understanding carbs can make a real difference in your daily life.
Why Carbs Matter for Blood Sugar
When you eat carbs-like bread, rice, fruit, or milk-they break down into glucose, which enters your bloodstream. That’s normal. But if your body doesn’t make enough insulin (type 1 diabetes) or doesn’t use it well (type 2 diabetes), that glucose stays in your blood too long, spiking your numbers. Carb counting helps you predict those spikes so you can match them with the right amount of insulin or adjust your meal timing.The American Diabetes Association (ADA) and the CDC both say carb counting works. Studies show people who track their carbs regularly see their HbA1c drop by 0.5% to 1.0% over time. That’s not just a number-it means fewer headaches, less fatigue, and lower risk of long-term damage to your eyes, kidneys, and nerves.
What Counts as One Carb Serving?
Carbs are measured in grams. One standard serving equals about 15 grams of total carbohydrates. That might sound vague, but here’s what it looks like in real life:- 1 small apple (about the size of a tennis ball)
- 1 slice of whole wheat bread
- 1/2 cup of cooked oatmeal
- 1/2 cup of cooked rice or pasta
- 1 cup of milk or plain yogurt
- 1/2 cup of beans or corn
These are your building blocks. Most adults with type 1 diabetes aim for 150-250 grams of carbs per day. That’s roughly 10-17 servings. But there’s no one-size-fits-all number. Your target depends on your weight, activity level, insulin sensitivity, and goals. Work with your doctor or a Certified Diabetes Care and Education Specialist (CDCES) to find your personal range.
How to Read Nutrition Labels Like a Pro
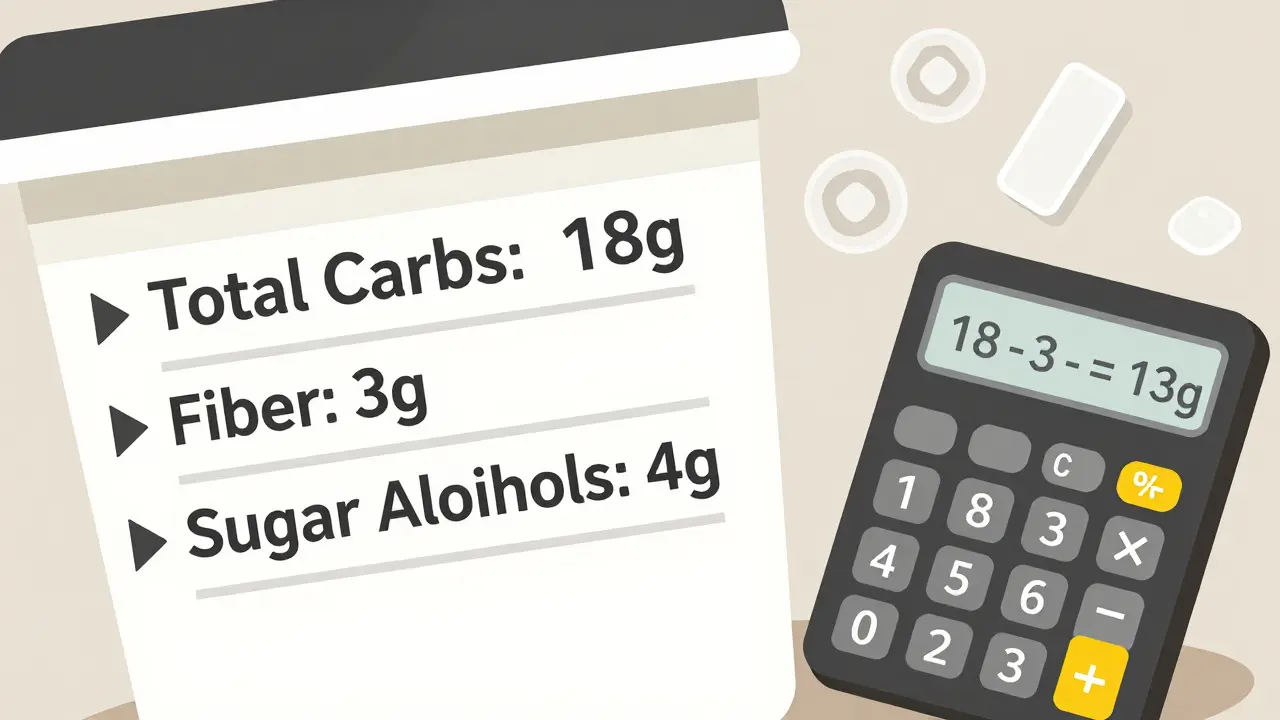
Look at the nutrition facts panel. Ignore the “sugars” line. Focus on total carbohydrates. That number includes starches, sugars, and fiber-all of it counts toward your carb total.But here’s the trick: you can subtract fiber and sugar alcohols under certain conditions.
- Fiber: If a food has 5 or more grams of fiber per serving, subtract the full amount. Fiber doesn’t raise blood sugar because your body doesn’t digest it.
- Sugar alcohols: These are found in sugar-free candies, gum, and some protein bars. Subtract half the grams listed. For example, if a bar has 10 grams of sugar alcohols, subtract 5 grams from the total carbs.
Example: A yogurt label says 18g total carbs, 3g fiber, and 4g sugar alcohols. You’d calculate: 18 - 3 - 2 = 13g net carbs.
Carb-to-Insulin Ratio: The Key to Matching Doses
If you take insulin, carb counting becomes even more powerful because you can match your dose to what you eat. That’s where the carb-to-insulin ratio comes in.This ratio tells you how many grams of carbs one unit of insulin covers. For example:
- A 1:10 ratio means 1 unit of insulin covers 10 grams of carbs.
- A 1:15 ratio means 1 unit covers 15 grams.
Your ratio isn’t the same for every meal. Most people need more insulin at dinner than breakfast because of how your body responds to insulin at different times of day. Your doctor or diabetes educator will help you figure this out. It often takes a few weeks of testing and adjusting.
Let’s say you’re eating a sandwich with 45g of carbs and your ratio is 1:10. You’d take 4.5 units of insulin (45 ÷ 10 = 4.5). Many insulin pens let you dial in half-units, so this is doable.
Carb Counting vs. Other Methods
You’ve probably heard of the plate method or the glycemic index. Here’s how carb counting stacks up:| Method | How It Works | Best For | Limitations |
|---|---|---|---|
| Carb Counting | Measuring exact grams of carbs; matching to insulin | People on insulin, especially pumps or multiple daily injections | Requires time, tools, and practice; can be overwhelming at first |
| Plate Method | Fill half your plate with non-starchy veggies, quarter with protein, quarter with carbs | Beginners, people not on insulin, simple lifestyle change | No precise numbers; harder to match insulin doses |
| Glycemic Index (GI) | Focusing on low-GI foods (like lentils, oats) that raise blood sugar slowly | People wanting to reduce spikes without insulin | Doesn’t tell you how much to eat; high-GI foods can still be healthy in small amounts |
Carb counting gives you the most control-if you’re willing to put in the work. If you’re not on insulin, the plate method might be easier to start with. But if you’re using insulin, carb counting is the gold standard.
What You Need to Get Started
You don’t need fancy gear, but these tools make it way easier:- A food scale (for accuracy with meats, cheese, and cooked grains)
- Measuring cups and spoons
- A reliable app: MyFitnessPal, Carb Manager, or the USDA’s FoodData Central
- A notebook or digital log to track meals and blood sugar readings
Start by logging everything you eat for 3 days. Don’t change anything-just record portions and carb counts. This gives you a baseline. Then, begin adjusting one meal at a time. Maybe start with breakfast. Once you feel confident, move to lunch, then dinner.
Common Mistakes Beginners Make
Even people who’ve read the guides still trip up. Here are the top errors:- Forgetting hidden carbs: Milk in coffee, yogurt in smoothies, sauces, and dressings all add up. Tomato sauce? 10g per 1/2 cup. Salad dressing? Up to 5g per tablespoon.
- Guessing restaurant meals: A “small” order of fries might have 45g of carbs-not the 30g you assumed. Chain restaurants often post nutrition info online. Use it.
- Not counting all carbs: Fruit, beans, and starchy veggies (like potatoes and peas) are healthy-but they still raise blood sugar. Don’t skip them just because they’re “good.”
- Ignoring fiber and sugar alcohols: That “sugar-free” granola bar might have 20g of carbs, but if it has 10g fiber and 6g sugar alcohols, your net is only 4g.
One study found that 25% of daily carb intake comes from unexpected sources like dairy and starchy vegetables. Keep a close eye on those.
Real-Life Success Stories
People on Reddit’s r/diabetes community report big wins after sticking with carb counting for a few weeks:- One user went from post-meal spikes of 250+ down to 160-180 within two weeks.
- A Type 1 patient lowered their HbA1c from 8.9% to 6.2% over 18 months by pairing carb counting with insulin adjustments.
- Another said they could finally enjoy pizza night without guilt-because they knew exactly how much insulin to take.
It’s not magic. It’s math. And it’s doable.

How Long Until You Get Good at It?
Don’t expect perfection on day one. Most people need 4 to 8 weeks to feel confident. The first month is the hardest-you’ll spend 30 to 60 minutes per meal measuring, logging, and calculating. That’s normal.After 30 days of consistent tracking, most people reach 85% accuracy in estimating carbs. That’s enough to make real improvements in blood sugar control. Use apps to speed things up. Carb Manager’s SmartScan feature, for example, lets you take a photo of your food and gets you a carb estimate with 85% accuracy.
When Carb Counting Might Not Be Right for You
Not everyone needs this level of detail. If you manage type 2 diabetes with diet and oral meds like metformin, you might do fine with the plate method or simply cutting back on processed carbs. Carb counting is most helpful when you’re using insulin-especially multiple daily injections or a pump.According to the 2023 National Health and Nutrition Examination Survey, only 32% of people with type 2 diabetes on oral meds practice formal carb counting. That’s because they don’t need to match insulin doses. But if your doctor suggests it, give it a shot. You might be surprised by how much better your numbers get.
The Future of Carb Counting
Technology is making carb counting smarter. Continuous glucose monitors (CGMs) now show you in real time how your blood sugar reacts to specific meals. That feedback loop is gold. If your glucose spikes after 15g of rice, you’ll know it’s not the right carb for you-even if the label says it’s “healthy.”Researchers are also testing systems where your insulin pump automatically adjusts doses based on what you scan or log. At Harvard’s Joslin Diabetes Center, early trials show these “closed-loop” systems can reduce HbA1c even further by syncing carb intake with insulin delivery.
And the ADA now emphasizes not just carb quantity, but quality. Whole grains, legumes, fruits, and non-starchy vegetables are preferred over white bread, sugary cereals, and pastries. You can still enjoy treats-but make the majority of your carbs nutrient-rich.
Do I have to count carbs forever?
You don’t have to count every gram for life, but you’ll always need to be aware of how much you’re eating. After a few months, you’ll start recognizing portion sizes by sight. A fistful of rice? About 15g. A banana? Around 27g. It becomes second nature. Think of it like learning to drive-you check the speedometer at first, then you just know.
Can I eat sugar if I count carbs?
Yes. Sugar is a carb, so it’s included in your total. A cookie with 20g of carbs counts the same as 20g of pasta. The difference is nutrition: pasta gives you fiber and minerals, while a cookie gives you mostly sugar and fat. You can enjoy the cookie-but balance it with better carbs elsewhere in your day.
What if I eat out and don’t know the carb count?
Most chain restaurants list nutrition info online. For local places, estimate based on similar dishes. A grilled chicken burrito? Think 50-60g carbs. A plate of spaghetti? 60-80g. Use apps like MyFitnessPal to find closest matches. When in doubt, choose a salad with protein and skip the bread. It’s better to be slightly conservative than to guess too high.
Do I need to count fiber and sugar alcohols every time?
If the food has 5 or more grams of fiber, yes-subtract it. Sugar alcohols should be halved and subtracted if they’re listed. Many packaged foods make it easy by showing “net carbs.” But always check the total carbs and ingredients list. Some brands use sugar alcohols to make a product seem lower-carb than it really is.
Can carb counting help me lose weight?
It can. Many people naturally eat fewer carbs when they start counting because they become aware of how much is in processed foods. But carb counting isn’t a weight-loss diet-it’s a blood sugar tool. If you want to lose weight, combine it with portion control and regular activity. Focus on whole foods, and you’ll likely lose fat without feeling deprived.
Next Steps: What to Do Today
You don’t need to overhaul your life. Start small:- Download a free app like MyFitnessPal or Carb Manager.
- Take a photo of your next meal and log the carbs.
- Check the nutrition label on one food item you eat daily-milk, cereal, or yogurt-and write down the total carbs.
- Call your doctor or diabetes educator and ask: “What’s my carb-to-insulin ratio?”
- Set a goal: “I will count carbs for breakfast for the next 7 days.”
Progress isn’t about perfection. It’s about consistency. One meal at a time, you’ll build confidence-and better control over your diabetes.

Nader Bsyouni
December 22, 2025 AT 04:24Why are we letting Big Pharma dictate our relationship with food? The real issue is insulin resistance from processed oils and sedentary lifestyles. Counting grams is like counting grains of sand on a beach while the tide rises.
Also, fiber doesn't 'not raise blood sugar'-it just delays it. You're being manipulated by nutrition labels that lie through omission.
Julie Chavassieux
December 23, 2025 AT 04:03Tarun Sharma
December 23, 2025 AT 11:18Herman Rousseau
December 25, 2025 AT 01:18Pro tip: Use Carb Manager’s barcode scanner-it’s a game changer. You got this!
Vikrant Sura
December 25, 2025 AT 08:50Candy Cotton
December 25, 2025 AT 23:42Jeremy Hendriks
December 27, 2025 AT 17:06But hey, keep counting your rice. Maybe that'll distract you from the fact that your life is being monetized.
Ajay Brahmandam
December 28, 2025 AT 00:59jenny guachamboza
December 29, 2025 AT 10:33