Beta-Lactam Allergies: Penicillin vs Cephalosporin Reactions Explained

Penicillin Allergy Assessment Tool
Based on scientific evidence, most people labeled as penicillin-allergic can safely take penicillin. This tool helps determine if your reaction was likely a true allergy or something else. Remember: A true allergy is IgE-mediated with rapid symptoms like hives, swelling, or breathing problems within 1 hour.
Your results will include evidence-based recommendations about whether you might be able to take penicillin or cephalosporins safely. Always consult a healthcare provider before changing your medication.
More than 10% of people in the U.S. say they’re allergic to penicillin. But here’s the truth: most of them aren’t. If you were told you’re allergic to penicillin as a kid after a rash from a virus, you might still be avoiding it today-even though you can probably take it safely. The same confusion extends to cephalosporins like ceftriaxone and cephalexin. Doctors often treat these two antibiotics as if they’re equally risky, but the science says otherwise.
What Exactly Is a Beta-Lactam Allergy?
Beta-lactam antibiotics include penicillins (like amoxicillin and penicillin V) and cephalosporins (like cefdinir and cefazolin). They all share a core chemical structure called the beta-lactam ring. That’s why people assume if you’re allergic to one, you’re allergic to all. But allergies aren’t about the ring alone-they’re about how your immune system reacts to specific side chains attached to it.
Penicillin allergies are the most commonly reported drug allergy in the U.S. But studies show that 90-95% of people labeled as allergic can tolerate penicillin after proper testing. Why? Because many reactions were never true allergies. A rash from a viral infection like mononucleosis? A headache after taking amoxicillin? These get labeled as “allergies” without testing-and stick for life.
Penicillin Reactions: What Actually Happens
True penicillin allergies are IgE-mediated. That means your body makes antibodies that trigger a rapid immune response. Symptoms show up within minutes to an hour after taking the drug:
- Hives (urticaria) in about 90% of cases
- Swelling of lips, tongue, or throat (angioedema) in half of cases
- Wheezing or trouble breathing in 30%
- Anaphylaxis-low blood pressure, shock, cardiac arrest-in 0.01% to 0.05% of doses
Most reactions are mild. But even mild ones get overblown. A 2022 Mayo Clinic study found that 65% of patients with a decades-old penicillin label could safely take penicillin after testing. Many of them had never seen an allergist. They just avoided it because their chart said “allergic.”
Cephalosporins: The Myth of High Cross-Reactivity
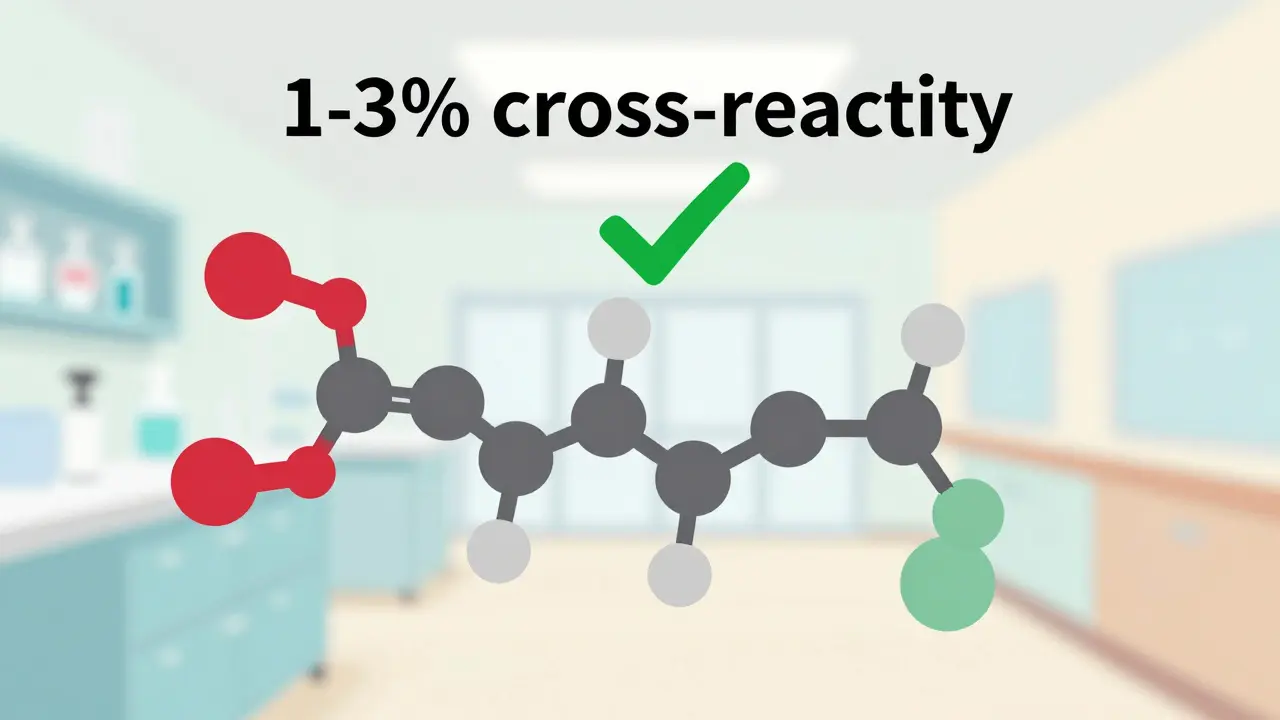
For years, doctors were taught that 10-30% of penicillin-allergic patients would react to cephalosporins. That number is outdated. Modern research shows the real cross-reactivity rate is closer to 1-3%-and even lower for later-generation cephalosporins.
Why? Because first-generation cephalosporins (like cefazolin) have side chains similar to penicillin. But third-generation ones (like ceftriaxone and cefdinir) are structurally different. Their side chains barely resemble penicillin’s. That’s why the CDC now says: “In most clinical settings, patients with reported penicillin allergy can safely receive ceftriaxone.”
Still, many hospitals won’t give cephalosporins to anyone with a penicillin allergy label. It’s not based on science-it’s based on habit. And that habit leads to worse outcomes. When patients are denied cephalosporins, they get alternatives like vancomycin or clindamycin. Those drugs are broader-spectrum, more expensive, and increase the risk of C. difficile infections by up to 30%.
Testing for Allergy: How It Really Works
If you think you’re allergic to penicillin, here’s what you should do:
- Get your history reviewed. Was it a rash? When? Did you have a fever? Was it after a virus? If it was a mild rash more than a year ago, you’re likely not allergic.
- Do skin testing. This is the gold standard. A small amount of penicillin (major and minor determinants) is pricked into your skin. If nothing happens, you’re likely not allergic. The test has a 97-99% negative predictive value.
- Do an oral challenge. If skin testing is negative, you’ll take a small dose of amoxicillin under observation. If you’re still fine after 1-2 hours, you’re cleared.
For cephalosporins? No standardized skin test exists. Commercial reagents aren’t widely available. So if you need a cephalosporin and have a penicillin label, doctors often skip testing and go straight to an oral challenge-especially with third-generation drugs.
What Happens If You Need Penicillin But Are Allergic?
Some infections only respond to penicillin. Think syphilis in pregnancy, neurosyphilis, or severe strep throat in high-risk patients. If you’re truly allergic, you can’t just skip it.
That’s where desensitization comes in. It’s not a cure. It’s a temporary reset. Under close supervision in a hospital, you get tiny, gradually increasing doses of penicillin every 15-30 minutes over 4-8 hours. Your immune system gets tricked into tolerating it. Success rates? Over 80%. It’s safe, effective, and used routinely in places like Mayo Clinic and Johns Hopkins.
But here’s the catch: it requires a monitored setting. You need IV access, epinephrine on hand, and staff trained for anaphylaxis. It’s not done in clinics. It’s done in hospitals.

Why This Matters More Than You Think
Every time a patient with a false penicillin allergy gets a broad-spectrum antibiotic instead of amoxicillin, it costs the system $2,000-$4,000 more per person annually. That’s because alternatives are pricier, require longer hospital stays, and cause more side effects.
And the health risks? Real. A CDC analysis found that patients with unverified penicillin allergy labels had 30% higher rates of surgical site infections because they couldn’t get the best preventive antibiotics. They also had higher rates of C. difficile infections-often deadly in older adults.
Hospitals that launched formal allergy delabeling programs saw:
- 23% drop in broad-spectrum antibiotic use
- 17% reduction in C. difficile cases
- Lower costs and better outcomes
Yet only 35% of U.S. hospitals have these programs. Most still rely on outdated charts and fear-based protocols.
What Should You Do?
If you’ve been told you’re allergic to penicillin:
- Don’t assume it’s true-especially if the reaction was a rash years ago.
- Ask your doctor if you can be referred to an allergist for testing.
- If you need antibiotics for an infection, ask: “Could I take amoxicillin or cefdinir instead?”
- If you’re pregnant or have syphilis, insist on evaluation-penicillin is the only safe option.
If you’re a clinician:
- Don’t just copy-paste “penicillin allergy” from old charts.
- Ask: “What was the reaction? When? Did it involve breathing or swelling?”
- Use the 2021 CDC guidelines. They’re clear: low-risk history? Skip skin testing. Go straight to oral challenge.
There’s no reason to keep people away from safe, effective antibiotics out of fear. Science has moved on. It’s time medicine caught up.
Can I outgrow a penicillin allergy?
Yes. About 80% of people who had a true penicillin allergy lose their sensitivity after 10 years. That’s why even if you were told you were allergic as a child, you should be retested if you need penicillin later in life. Skin testing and oral challenges can confirm whether you’re still allergic.
Is it safe to take cephalosporins if I’m allergic to penicillin?
For most people, yes. The risk of cross-reactivity is only 1-3%, and it’s even lower with third-generation cephalosporins like ceftriaxone or cefdinir. The outdated belief that 10-30% of penicillin-allergic patients react to cephalosporins has been debunked by modern studies. If you need a cephalosporin and have a penicillin label, ask your doctor about an oral challenge-no skin test is needed for many cases.
What’s the difference between a side effect and a true allergy?
A side effect isn’t an immune response. Nausea, diarrhea, or a mild rash from a virus aren’t allergies. A true IgE-mediated allergy causes hives, swelling, trouble breathing, or low blood pressure within minutes to an hour. If your reaction was delayed (more than 24 hours) or didn’t involve breathing or swelling, it’s likely not a true allergy. Documenting the exact symptoms helps future providers make better decisions.
Can I take amoxicillin if I had a rash after penicillin as a kid?
Probably. Many childhood rashes after penicillin were caused by viruses like Epstein-Barr, not the drug. If the rash was mild, didn’t involve swelling or breathing issues, and happened more than a year ago, you’re likely not allergic. A simple oral challenge with amoxicillin under medical supervision can confirm this safely-and quickly.
Why don’t all hospitals test for penicillin allergy?
Because it takes time, training, and resources. Skin testing requires allergists, specific reagents, and monitoring equipment. Only 28% of rural hospitals have access to allergists. And many providers still believe the old 10-30% cross-reactivity myth. But hospitals with formal programs-like Mayo Clinic and Johns Hopkins-have shown they can safely delabel 60-70% of patients, cut antibiotic costs, and reduce infections. It’s not about lack of knowledge-it’s about lack of systems.

Brad Ralph
February 13, 2026 AT 07:11christian jon
February 13, 2026 AT 15:32Suzette Smith
February 15, 2026 AT 03:07Autumn Frankart
February 16, 2026 AT 13:25Skilken Awe
February 17, 2026 AT 12:48andres az
February 18, 2026 AT 14:52Steve DESTIVELLE
February 19, 2026 AT 14:36Stephon Devereux
February 19, 2026 AT 21:09steve sunio
February 21, 2026 AT 17:52Neha Motiwala
February 22, 2026 AT 05:08athmaja biju
February 22, 2026 AT 20:16Robert Petersen
February 24, 2026 AT 03:00Craig Staszak
February 24, 2026 AT 15:12Stephon Devereux
February 25, 2026 AT 09:37alex clo
February 26, 2026 AT 04:53