Beta-Blockers and Calcium Channel Blockers: What You Need to Know About Combination Therapy
Beta-Blocker & CCB Safety Checker
Check Your Combination Safety
This tool helps determine if a specific beta-blocker and calcium channel blocker combination is safe for you based on current clinical guidelines.
When your heart is working too hard, doctors often turn to beta-blockers or calcium channel blockers to slow it down. But what happens when you use both? This combination isn’t just adding two drugs together-it’s mixing two powerful forces that can either help your heart or push it too far. Many patients get this combo for high blood pressure or chest pain, especially when one drug alone isn’t enough. But the risks? They’re real, and not everyone knows about them.
How These Drugs Work-And Why They’re Combined
Beta-blockers, like metoprolol and atenolol, work by blocking adrenaline’s effect on the heart. This lowers heart rate, reduces blood pressure, and decreases how hard the heart pumps. Calcium channel blockers, such as amlodipine and diltiazem, relax blood vessels by stopping calcium from entering muscle cells. That also lowers blood pressure and can ease chest pain.
Together, they hit the heart from two angles. One slows the rhythm, the other relaxes the pipes. That’s why they’re often used for patients with both high blood pressure and angina. For some, this combo controls symptoms better than either drug alone. But here’s the catch: not all calcium channel blockers are the same. And mixing the wrong one with a beta-blocker can be dangerous.
The Big Divide: Dihydropyridines vs. Non-Dihydropyridines
Not all calcium channel blockers are created equal. There are two main types: dihydropyridines (like amlodipine and nifedipine) and non-dihydropyridines (like verapamil and diltiazem). The difference matters a lot when paired with beta-blockers.
Dihydropyridines mostly affect blood vessels. They don’t slow the heart much on their own. So when you add a beta-blocker, the heart rate drops-but not dangerously so. Studies show that beta-blockers and amlodipine are well-tolerated in most patients. One 2023 study of over 18,000 people found this combo lowered stroke risk by 22% and heart failure risk by 28% compared to other dual therapies.
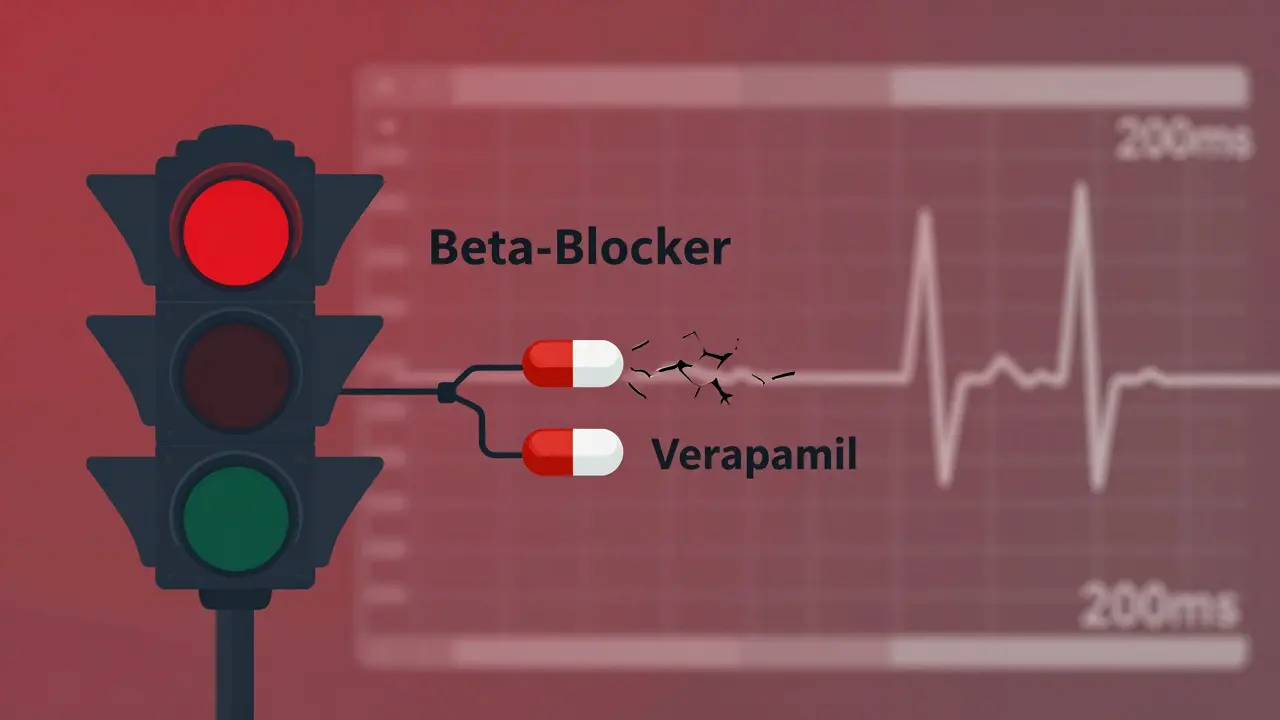
Non-dihydropyridines, though, hit the heart directly. Verapamil and diltiazem slow electrical signals and reduce how strongly the heart contracts. When you combine them with beta-blockers, you’re essentially double-blocking the heart’s natural pace. That’s where things go wrong.
The Hidden Danger: When the Heart Slows Too Much
Imagine your heart’s electrical system as a traffic light. Beta-blockers make the green light shorter. Verapamil makes it turn yellow even faster. Together? The light turns red-and stays that way. That’s what happens in some patients.
Research shows that beta-blockers plus verapamil cause dangerous bradycardia (heart rate under 50 bpm) or heart block in 10-15% of patients. In older adults, the risk jumps even higher. One study found a 3.2-fold increase in pacemaker implantations with this combo compared to beta-blockers plus amlodipine. There are real stories behind these numbers: a Reddit thread from a cardiologist described losing a patient to complete heart block after adding verapamil to metoprolol in an 82-year-old with a borderline PR interval. That’s not a rare case-it’s a warning.
Doctors now check the PR interval on an ECG before prescribing this combo. If it’s over 200 milliseconds, guidelines say: don’t do it. The European Society of Cardiology explicitly bans verapamil with beta-blockers in patients with sinus node dysfunction or existing heart block. Yet, some clinicians still use it, especially if they think the patient “needs it.” That’s where things get risky.
Who Benefits? Who Should Avoid It?
This combo isn’t for everyone. But it’s not useless either. The best candidates are patients with:
- Hypertension and stable angina
- Resting heart rate above 80 bpm (beta-blockers help here)
- No history of heart failure with reduced ejection fraction
- No pre-existing conduction problems
Who should avoid it entirely?
- Patients with second- or third-degree heart block
- Those with sick sinus syndrome
- People with ejection fraction under 45%
- Anyone over 75 with untested conduction system
- Those already on other heart-slowing meds (like digoxin)
And here’s something many don’t realize: even safe combos can cause side effects. Peripheral edema-swelling in the ankles-is common with dihydropyridines. About 22% of patients on beta-blocker + amlodipine get it. That’s higher than with other combos. But it’s usually manageable with a lower dose. Verapamil combos? They cause 2.3 times more people to quit the medication because of side effects.
What Doctors Do Before Prescribing
Good clinicians don’t just write a prescription. They check. They measure. They plan.
Before starting this combo, most guidelines require:
- An ECG to check PR interval and heart rhythm
- An echocardiogram to measure ejection fraction
- Review of all other medications (especially if the patient takes digoxin or antiarrhythmics)
After starting, patients are monitored closely. Heart rate and blood pressure are checked weekly for the first month. Some clinics use an online risk calculator developed by the European Society of Cardiology-it’s 89% accurate at predicting who might develop dangerous bradycardia.
One hospital system, Kaiser Permanente, reduced adverse events by 44% after implementing standardized protocols in 2020. That’s not magic-it’s discipline. And it’s something every provider should follow.
What the Data Says About Long-Term Outcomes
Is this combo worth it? The data says: sometimes.
A 2023 study of 18,681 Chinese patients found beta-blocker + dihydropyridine CCB combinations reduced major heart events by 17% and heart failure by 28%. That’s better than ACE inhibitors plus CCBs. But the same study showed beta-blocker + verapamil increased heart failure hospitalizations by 2.8 times. The difference? One is a safe pair. The other is a ticking clock.
The American Heart Association now recommends avoiding verapamil with beta-blockers in older adults. The FDA added a boxed warning in 2021. The European Medicines Agency now requires an echocardiogram before prescribing the combo. These aren’t small changes-they’re red flags.
And yet, the market is shifting. In the U.S., only 12% of dual therapy prescriptions are beta-blocker + CCB. In China, it’s 22%. Why? Because Chinese guidelines still include it more broadly. But even there, doctors are starting to favor amlodipine over verapamil.
Real Talk From the Front Lines
Doctors aren’t just reading guidelines-they’re living them.
Dr. Sarah Chen, a cardiologist in Boston, says she’s prescribed beta-blocker + amlodipine to over 200 patients. Only 3% developed ankle swelling, and lowering the dose fixed it. “It’s reliable,” she says. “I use it when the patient needs both heart rate control and blood pressure reduction.”
But another doctor on a medical forum shared a different story: “I avoided verapamil with beta-blockers after a 78-year-old went into full heart block. His PR was 210ms. We missed it. He didn’t survive.” That’s the kind of story that changes practice.
When surveyed, 78% of U.S. clinicians prefer beta-blocker + dihydropyridine combos. Only 12% would even consider verapamil. And 63% say their biggest fear is bradycardia. That’s not paranoia-it’s experience.
What’s Next for This Therapy?
The future isn’t about expanding this combo. It’s about narrowing it.
Research is moving toward risk stratification tools. The European Society of Hypertension is testing a new algorithm to predict who’s safe for this therapy. Early results look promising. Industry analysts predict beta-blocker + dihydropyridine prescriptions will grow 5.7% per year through 2028-mostly because they’re safer.
Verapamil combinations? They’re fading. Not because they don’t work-but because the risks outweigh the benefits for most patients. The goal now isn’t to use more combos. It’s to use the right ones, in the right people, with the right checks.
Bottom Line: It’s Not About Both Drugs-It’s About Which One
If your doctor suggests beta-blockers and calcium channel blockers together, ask: Which one? Amlodipine? Or verapamil?
One is a safe, effective option for many. The other is a high-risk choice that should only be used in rare cases-and even then, with extreme caution. Never assume “more drugs = better results.” In this case, the wrong combination can be life-threatening.
Make sure your doctor checks your ECG. Ask about your heart’s pumping strength. Know your PR interval. And if you’re over 65, don’t let them skip the echocardiogram. This isn’t just about controlling blood pressure-it’s about protecting your heart from the very drugs meant to help it.
Can beta-blockers and calcium channel blockers be taken together safely?
Yes-but only under strict conditions. Beta-blockers paired with dihydropyridine calcium channel blockers like amlodipine are generally safe and effective for hypertension and angina. However, combining beta-blockers with non-dihydropyridines like verapamil or diltiazem can cause dangerous drops in heart rate or heart block, especially in older adults or those with pre-existing conduction issues. Always get an ECG and echocardiogram before starting this combo.
Which calcium channel blocker is safest with beta-blockers?
Amlodipine, a dihydropyridine calcium channel blocker, is the safest option when combined with beta-blockers. It mainly relaxes blood vessels without significantly slowing heart rate or conduction. Verapamil and diltiazem, non-dihydropyridines, strongly affect the heart’s electrical system and should be avoided with beta-blockers in most patients, especially those over 65 or with any history of slow heart rhythms.
What are the signs that this combination is causing problems?
Watch for dizziness, extreme fatigue, fainting, shortness of breath, or a pulse under 50 beats per minute. Swelling in the ankles is common with amlodipine but usually mild. Sudden drops in heart rate or irregular heartbeat could signal dangerous heart block. If you notice any of these, contact your doctor immediately. Don’t wait for your next appointment.
Do I need an ECG before starting this combo?
Yes. Guidelines from the European Society of Cardiology and the American Heart Association require a baseline ECG to check your PR interval and heart rhythm. If your PR interval is over 200 milliseconds, this combo is contraindicated. Many doctors skip this step, but it’s critical. A simple 10-second test can prevent life-threatening complications.
Is this combination still commonly prescribed?
In the U.S., it’s used in about 12% of dual therapy prescriptions for hypertension-third behind ACE inhibitor + CCB and ACE inhibitor + thiazide. Its use is declining for verapamil combinations due to safety concerns. Amlodipine-based combos are still common, especially for patients with angina and high heart rate. But overall, doctors are becoming more selective, preferring safer alternatives unless the patient has clear, documented benefit.
Can this combo cause heart failure?
Yes, especially with verapamil. Studies show beta-blocker + verapamil combinations increase the risk of heart failure hospitalization by nearly three times compared to beta-blocker + amlodipine. This is because verapamil reduces the heart’s pumping strength, and beta-blockers further suppress it. In patients with already weakened hearts (ejection fraction below 45%), this combo can be dangerous. Always know your ejection fraction before starting.

Chris & Kara Cutler
February 2, 2026 AT 11:34This combo saved my dad’s life after his angina got worse. Amlodipine + metoprolol, no issues. Just watch for swollen ankles - we fixed it with a lower dose.
Rachel Liew
February 3, 2026 AT 22:04i read this and thought about my grandma who got put on verapamil and then passed out at the grocery store. they never checked her pr interval. she was 79. this needs to be louder.
Nicki Aries
February 4, 2026 AT 20:40Wait, so you’re saying the FDA and ESC are now basically saying: ‘Don’t mix verapamil with beta-blockers unless you’re willing to risk a pacemaker?’ That’s huge. I’ve seen so many patients on this combo because their doc ‘didn’t think it was a big deal.’
And honestly? That’s the problem. Medicine still operates on habit, not data. This post should be required reading for every med student and every GP who writes scripts for hypertension.
Lisa Rodriguez
February 5, 2026 AT 16:00My clinic just started using that ESC risk calculator and it’s been a game changer. We used to just eyeball PR intervals. Now we plug in age, meds, ejection fraction - it tells us if the combo’s a yes or a hard no. Saved two people from complete heart block last month alone.
Also - yes, amlodipine causes ankle swelling. But it’s way better than dying. And diuretics help. Don’t let that scare you off the right combo.
Ishmael brown
February 5, 2026 AT 18:27So you’re telling me the ‘safe’ combo causes swelling, and the ‘dangerous’ one causes death - but we’re still pushing the swelling one because it’s less likely to kill you immediately?
That’s not safety. That’s just damage control. We’re treating symptoms instead of fixing the system. This whole approach is broken.
Nidhi Rajpara
February 6, 2026 AT 12:56Actually, in India, we use verapamil + beta-blocker quite often - especially in rural areas where ECG machines are rare. We rely on pulse checks and patient reports. It’s not ideal, but it’s what we have. Maybe we need better infrastructure, not just stricter guidelines.
Deep Rank
February 8, 2026 AT 02:26Oh wow, so now we’re supposed to fear verapamil like it’s a villain in a superhero movie? Meanwhile, the real problem is that doctors don’t listen to patients. My aunt had bradycardia for months and nobody checked her ECG because she ‘looked fine.’
And now you want us to believe that amlodipine is the hero? It gave her swollen legs so bad she couldn’t walk. So now she’s on diuretics, which made her dizzy, and then they added potassium, which made her nauseous. So what’s the win here?
Everyone’s just swapping one side effect for another. Nobody’s asking: why are we even giving two heart-slowing drugs to someone who just needs to walk to the bathroom without passing out?
This isn’t medicine. It’s pharmaceutical roulette.
Aditya Gupta
February 9, 2026 AT 22:49my uncle on this combo for 5 years. no issues. amlodipine + bisoprolol. he walks 10k steps daily. no swelling. no dizziness. maybe the real issue is overtesting?
not everyone needs an echo. not everyone is 80.
Nancy Nino
February 11, 2026 AT 02:15How refreshing to see a post that doesn’t just say ‘take your meds’ but actually explains why the difference between amlodipine and verapamil is the difference between life and a very expensive funeral.
Thank you. Someone finally spoke plainly.
Ed Di Cristofaro
February 11, 2026 AT 21:02lol so doctors are scared of verapamil now? i bet they're also scared of coffee and stairs. you think your heart is fragile? mine's been through 3 heart attacks and a triple bypass. i'm on both. i'm 71. still ride my bike. you're overcomplicating this.
Lilliana Lowe
February 12, 2026 AT 13:57While your post is technically accurate, you’ve omitted the most critical point: the pharmacokinetic interactions between CYP3A4 substrates and beta-blockers metabolized via hepatic pathways. Without addressing metabolic clearance, you’re presenting a superficial risk profile. The real danger lies in polypharmacy with statins, antifungals, or grapefruit juice - which are rarely considered in these clinical summaries.
Furthermore, the 2023 Chinese study you cite was observational. It lacked adjustment for socioeconomic confounders, which heavily influence cardiac outcomes in that population. Your conclusion is premature at best.
Donna Macaranas
February 13, 2026 AT 03:47i just read this while waiting for my blood pressure check. i’m on amlodipine and metoprolol. my doc checked my ekg last week. i didn’t know why until now. thanks for explaining. feels good to know i’m not just a number.
vivian papadatu
February 13, 2026 AT 15:26I’ve been a nurse for 22 years, and I’ve seen the aftermath of this combo more times than I can count. I’ve held the hand of a woman who went into full heart block after her cardiologist added verapamil because her BP was still 150/95. She didn’t have a PR interval check. She didn’t have an echo. She was 74. She didn’t wake up.
And I’ve seen the same patient - same BP, same angina - put on amlodipine instead. She’s still here. Still gardening. Still complaining about her swollen ankles. But she’s here.
It’s not about being scared of drugs. It’s about being scared of being careless. Every time we skip the ECG because ‘she looks fine,’ we’re gambling with someone’s last breath. And we’re not just risking lives - we’re eroding trust. Patients don’t need more drugs. They need more care.
So yes, this post is long. But so is the list of people we’ve lost because we thought we knew better than the guidelines. This isn’t just medicine. It’s moral responsibility. And if you’re not checking PR intervals before prescribing this combo, you’re not a doctor. You’re a gambler with a stethoscope.
Jamie Allan Brown
February 14, 2026 AT 23:24My dad’s cardiologist told him the same thing - amlodipine over verapamil. He asked why. The doc pulled up the ESC guidelines on his tablet and said, ‘Because if we’re wrong, you might need a pacemaker. Or you might die. And I don’t want to explain that to your daughter.’
That’s the moment I realized: good doctors don’t just follow guidelines. They’re terrified of what happens when they don’t.